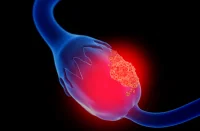
Hepatocellular carcinoma (HCC), the most common type of primary liver cancer, poses unique diagnostic and therapeutic challenges due to its complex biological behaviour. Intratumoural fat—fat deposits within the tumour tissue—has become an area of focus as it appears to be associated with different prognostic outcomes. MRI imaging has proven essential for non-invasive assessment, allowing detailed insights into fat patterns within tumours. However, the prognostic significance of intratumoural fat in HCC is debated. A recent review published in Radiology examines a comprehensive cohort study on general and homogeneous intratumoural fat roles in HCC, covering patient outcomes in both Asian and European contexts.
Intratumoural Fat in HCC: Clinical and Biological Insights
The presence of intratumoural fat in HCC reflects various biological processes, often linked to fatty degeneration, hypoxia and metabolic dysregulation. The development of fat within tumours can be attributed to metabolic conditions such as diabetes, obesity or fatty liver disease. However, these associations vary significantly by patient demographics and liver disease aetiologies, affecting tumour development and patient prognosis.
In this study, differences in fat patterns were analysed across two patient cohorts—one from East Asia, primarily associated with hepatitis B, and another from Western Europe, where metabolic dysfunction–associated fatty liver disease was more common. Fat-containing tumours in both cohorts often exhibited such characteristics as non-peripheral washout, enhancing capsules and mosaic architecture, all visible on MRI scans. However, a notable divergence was observed in fat frequency and impact across the cohorts. For Asian patients, intratumoural fat often aligned with the steatohepatitic subtype of HCC, showing a higher incidence of non-aggressive features. These results suggest that MRI-assessed intratumoural fat, while significant in both cohorts, may represent a complex of factors influenced by distinct underlying health conditions.
Comparing Homogeneous and Heterogeneous Intratumoural Fat Patterns
MRI assessment allows for further categorisation of intratumoural fat patterns into homogeneous (uniform) and heterogeneous (mixed) distributions. The study found that homogeneous intratumoural fat might be associated with more favourable tumour biology, particularly in Asian patients. Homogeneous fat distribution, which was identified in 15% of Asian patients and 14% of European patients, was linked with longer recurrence-free survival (RFS) and overall survival (OS) within the Asian cohort. These patients also exhibited lower incidences of vascular invasion and smaller tumours, which often translated into less aggressive tumour behaviour.
Conversely, heterogeneous fat patterns were frequently associated with increased tumour heterogeneity and less favourable outcomes, potentially due to the more chaotic distribution of fatty tissue within the tumour. This distribution may reflect a range of underlying biological pathways, such as the immune system's response to the tumour microenvironment, which can influence the effectiveness of treatments. Interestingly, homogeneous fat did not show similar prognostic associations in the European cohort, possibly due to differences in disease presentation or sample size. Nevertheless, homogeneous intratumoural fat presents a promising marker for prognosis in HCC, potentially guiding less aggressive treatment approaches for specific patient populations.
Implications for Personalised Treatment and Prognostic Assessment
MRI-assessed intratumoural fat holds substantial promise as a non-invasive imaging biomarker in HCC treatment planning, particularly for Asian patients with hepatitis B-related HCC. Clinicians might consider less intensive treatment strategies for patients presenting with homogeneous intratumoural fat, as these patients may experience favourable outcomes with conservative approaches. In contrast, the study found no significant difference in RFS and OS when analysing intratumoural fat in general. This underscores the importance of identifying specific fat patterns rather than relying on general fat presence as a prognostic indicator.
In both cohorts, patients with homogeneous intratumoural fat often presented with higher body mass index (BMI) and reduced markers of tumour aggression, such as lower rates of vascular invasion and smaller tumour size. MRI-assessed homogeneous intratumoural fat was further linked to reduced incidences of necrosis and haemorrhage within the tumour, factors commonly associated with aggressive cancer behaviour. These findings support the potential of homogeneous fat as a prognostic biomarker that may assist in tailoring treatments according to specific tumour profiles.
As with any emerging biomarker, further research is necessary to validate homogeneous intratumoural fat's predictive value across diverse patient populations. Additionally, challenges remain in achieving high interrater reliability in MRI assessments due to the subjective nature of current qualitative assessments. The integration of artificial intelligence and quantitative imaging approaches, such as MRI-derived proton density fat fraction, could improve diagnostic accuracy and consistency, making homogeneous intratumoural fat a more robust factor in clinical decision-making.
The study offers valuable insights into the prognostic value of MRI-assessed intratumoural fat patterns in HCC, especially in heterogeneous populations with varying disease aetiologies. Homogeneous intratumoural fat appears to correlate with improved survival outcomes in Asian patients, highlighting its potential as a valuable biomarker for guiding personalised treatment plans. However, regional and demographic differences underscore the need for a tailored approach to assessing intratumoural fat's prognostic relevance. Continued research and advancements in imaging technology will be essential in refining this biomarker’s application, potentially enhancing patient outcomes through more targeted, evidence-based treatment strategies.
Source: Radiology
Image Credit: iStock