A prospective diagnostic study provides a bridge between validating amyloid positron emission tomography (PET) in a research setting and implementing this diagnostic tool in daily clinical practice. Both amyloid-positive and amyloid-negative results had substantial associations with changes in diagnosis and treatment, both in patients with and without dementia, according to the study published online in JAMA Neurology.
"The etiological diagnosis changed for 25 percent of patients after amyloid PET, more often due to a negative than a positive PET result. Diagnostic confidence increased, and for several patients, there was a change in the treatment received by patients post-PET," the authors write. "Disclosing the amyloid PET results resulted in a decrease in uncertainty, whereas anxiety did not increase."
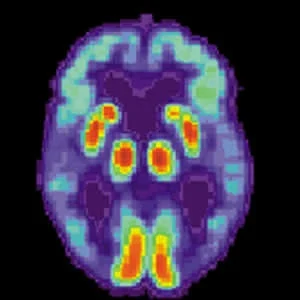
The accumulation of brain amyloid-β is one of the neuropathological hallmarks of Alzheimer disease (AD). The introduction of carbon 11–labelled Pittsburgh compound B ([11C]PIB) enabled the detection of brain amyloid-β deposition in vivo using PET. Amyloid PET has now been incorporated in research criteria for diagnosing AD. As a result, amyloid PET has gained a prominent role in research, although not yet in daily clinical practice
This study aimed to examine the association of amyloid PET with changes in diagnosis, diagnostic confidence, treatment, and patients’ experiences in an unselected memory clinic cohort (n=507). Participants underwent amyloid PET imaging as part of their routine diagnostic dementia workup. For each patient, neurologists determined a preamyloid and postamyloid PET diagnosis that existed of both a clinical syndrome (dementia, mild cognitive impairment, or subjective cognitive decline) and a suspected etiology (Alzheimer disease [AD] or non-AD), with a confidence level ranging from 0% to 100%. In addition, the neurologist determined patient treatment in terms of ancillary investigations, medication, and care. Each patient received a clinical follow-up one year after being scanned.
Of 507 patients, amyloid PET results were positive for 242 of them (48%). The suspected etiology changed for 125 patients (25%) after undergoing amyloid PET, more often due to a negative (82 of 265 [31%]) than a positive (43 of 242 [18%]) PET result (P < .01). Post-PET changes in suspected etiology occurred more frequently in patients older (>65 years) than younger (<65 years) than the typical age at onset of 65 years (74 of 257 [29%] vs. 51 of 250 [20%]; P < .05). Mean diagnostic confidence (SD) increased from 80 (13) to 89 (13%) (P < .001).
Moreover, in 123 patients (24%), there was a change in patient treatment post-PET, mostly related to additional investigations and therapy.
"Whether to disclose an amyloid PET result to patients with MCI [mild cognitive impairment] and cognitively normal individuals is controversial given the current lack of understanding of the predictive value of an amyloid PET result at an individual level," the authors point out. "In this study, we asked a subset of patients about their levels of anxiety and uncertainty before and after undergoing amyloid PET. Their levels of anxiety did not increase after disclosure, whereas their levels of uncertainty decreased, which was attributable to a decrease in uncertainty in patients for whom the neurologist disclosed the PET results."
These preliminary results indicate that amyloid PET result disclosure in a clinical setting does not seem harmful to patients in terms of anxiety or uncertainty, according to the authors.
Source: JAMA Neurology
Image Credit: Wikimedia Commons
References:
de Wilde A et al. (2018) Association of Amyloid Positron Emission Tomography With Changes in Diagnosis and Patient Treatment in an Unselected Memory Clinic Cohort: The ABIDE Project. JAMA Neurol. Published online June 11, 2018. doi:10.1001/jamaneurol.2018.1346
Latest Articles
Dementia, cognitive impairment, Amyloid PET
Amyloid PET improves evaluation of patients with cognitive impairment