HealthManagement, Volume 25 - Issue 3, 2025
Biokinetics is a patient-centred, evidence-based exercise therapy that enhances chronic disease management by improving function, reducing hospital readmissions and supporting long-term recovery. Despite being underutilised, it effectively complements pharmaceutical treatment and addresses the physical causes and symptoms of non-communicable diseases. Its integration into multidisciplinary care offers a holistic and cost-effective approach to global health challenges.
Key Points
- Biokinetics uses exercise therapy to manage and prevent chronic non-communicable diseases.
- It improves physical function, reduces symptoms and enhances quality of life for patients.
- Biokinetics supports cost-effective care by reducing hospital readmissions and promoting recovery.
- Despite its benefits, biokinetics remains underprescribed in chronic disease treatment.
- Integration with multidisciplinary teams ensures holistic and patient-centred care.
Introduction
Chronic non-communicable diseases (NCDs) like cardiovascular disease, diabetes, respiratory disease and musculoskeletal disorders are the main cause of disability and death worldwide. They need more than medication: they require sequential, continuous care interventions that optimise function and delay deterioration.
Biokinetics, a clinical South African-born profession, is an expert, evidence-based exercise intervention in prevention and rehabilitation. Biokineticists occupy a vital position at the intersection of physical medicine and long-term lifestyle management, particularly in chronically ill patients. Their contributions span clinical, economic and structural dimensions within modern health systems.
Epidemiology of Chronic Diseases and the Role of Biokineticists in their Management
NCDs are still the largest contributors to the world's mortality, disability and healthcare burden. NCDs cause more than 74% of deaths in the world, the lion's share being contributed by cardiovascular diseases (CVDs), cancer, chronic respiratory diseases and diabetes, according to the World Health Organisation (WHO). Table 1. demonstrates the figures accordingly.
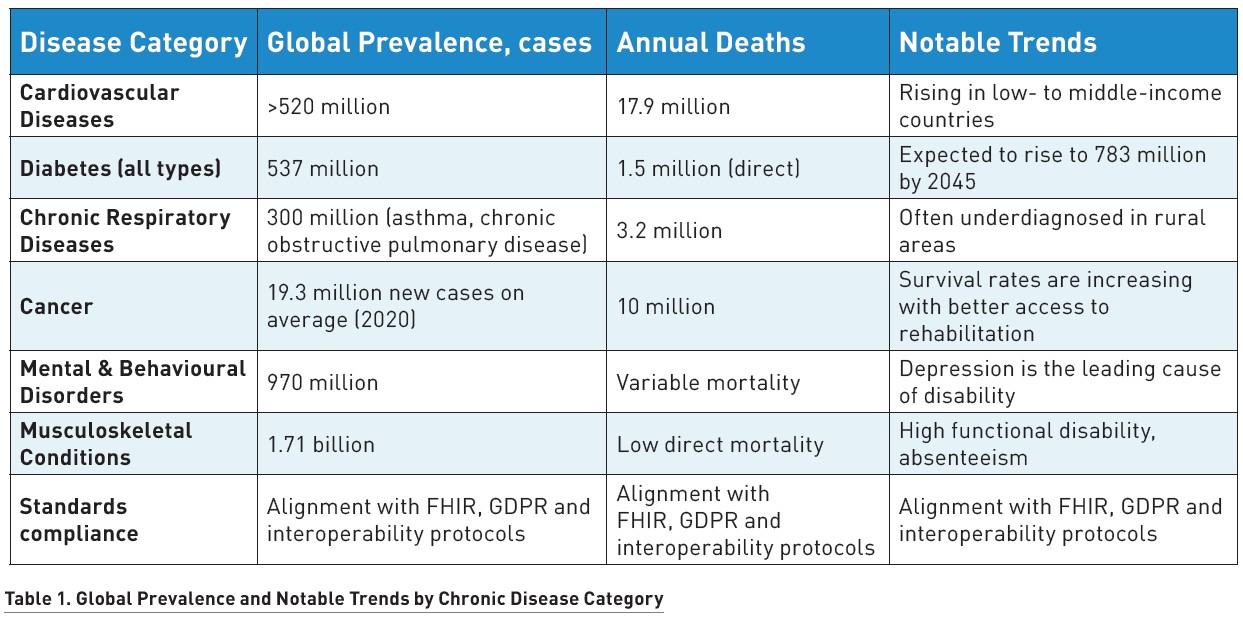
The burden of disease varies across different settings. In urban populations, NCDs are more prevalent due to lifestyle factors such as sedentary employment, poor diet and chronic stress. In contrast, rural and peri-urban populations face increased unmet healthcare needs, primarily due to limited access to diagnostics, rehabilitation and follow-up treatment.
Biokinetics in Practice & Utilisation Gaps
Biokinetics is a clinical science that addresses the functional and systemic consequences of chronic disease by applying goal-oriented, evidence-based physical rehabilitation. Its contribution most closely relates to four main global health objectives. In the first place, it prevents premature death due to NCDs through increased cardiorespiratory fitness, glycaemic control and mobility. Second, biokinetics is indispensable in maximising health-related quality of life by reducing chronic pain, fatigue and disability. Third, it minimises hospitalisation and readmission by maximising physical function and frequency and severity of disease exacerbation. Lastly, biokinetics adds to economic productivity by promoting functional independence and re-employment into the workforce.
Despite its clear benefits, biokinetics remains significantly underprescribed. Fewer than 15% of South African patients who qualify are referred to biokinetics following cardiac events. In managing NCDs, pharmacotherapy is typically the sole intervention, even though clinical guidelines recommend structured movement as part of treatment. Similarly, physical activity is rarely prescribed for mental health patients, despite evidence showing that exercise can produce effects comparable to antidepressants in certain mild to moderate conditions.
Aetiology of Chronic Disease and Implications for Biokinetics
The aetiology of most chronic diseases involves a multifaceted interaction between genetic predisposition, environment, lifestyle and socio-economic status. For instance:
- for cardiovascular diseases (CVDs), risk factors include high blood pressure, smoking, overweight, dyslipidaemia and physical inactivity;
- type 2 diabetes is strongly linked with physical inactivity, central obesity and poor dietary quality;
- osteoarthritis is often stimulated by joint loading patterns, age and previous injury.
Biokineticists operate at the level of disease causation, addressing the underlying physical factors that contribute to chronic conditions. Through guided movement prescription, they manage sedentary behaviour, impaired neuromuscular control, strength imbalances and maladaptive movement patterns—factors that form the basis of chronic disease onset and progression.
Pathophysiology and Functional Decline in Chronic Diseases
Most chronic diseases involve progressive dysfunction at the tissue, organ or system level, significantly affecting daily life. These include:
- Cardiovascular diseases: Progressive endothelial dysfunction and vascular stiffening impair cardiac efficiency;
- Respiratory diseases: Inflammation and obstruction of the airways limit oxygen supply;
- Musculoskeletal disorders: Degenerative and inflammatory processes compromise tissue elasticity and joint mobility.
This is quantified as measurable deficits in functional capacity, cardiovascular reserve, muscular strength and balance, as well as neurocognitive function. Biokineticists prescribe exercise as medicine to reverse or slow this process via structured loading, neural retraining and cardiovascular conditioning.
Clinical Signs and Symptoms During Chronic Illness
Chronic illness is not only identified through tests and scans but also through declines in mobility, function, energy and independence—areas in which biokineticists play a therapeutic role. Some of these clinical manifestations are listed below:
- Cardiovascular system: fatigue, dyspnoea, exercise intolerance;
- Metabolic system: poor glucose control, weight gain, fatigue;
- Respiratory system: breathlessness, reduced lung capacity;
- Musculoskeletal system: joint pain, stiffness, reduced range of motion;
- Neurological system: gait instability, coordination deficits and cognitive decline;
- Psychological system: depression, anxiety and lack of motivation.
Biokinetics helps the doctor by directly managing these symptoms, restoring function and gaining measurable improvements consistent with therapeutic objectives.
Pharmaceuticals & Biokinetics Synergy in Chronic Disease Management
Chronic disease management typically relies on a combination of pharmaceutical treatment, lifestyle interventions and rehabilitation. While medication is essential for controlling symptoms, slowing disease progression and preventing complications, biokinetics serves as a valuable adjunct therapy that can significantly improve treatment outcomes. The following paragraph outline major chronic diseases, the pharmaceutical classes commonly used in their management and the complementary role of biokinetics in enhancing clinical outcomes.
Cardiovascular Conditions
In cardiovascular diseases such as hypertension, coronary artery disease, heart failure, peripheral arterial disease and stroke, medications like ACE inhibitors, beta-blockers, diuretics, statins and antiplatelets help manage key physiological parameters. These treatments work to lower blood pressure, control angina, reduce clot formation and enhance cardiac output. Biokinetics complements these effects by improving vascular tone, reducing resting blood pressure, enhancing overall functional capacity and supporting natural antihypertensive responses.
In cases of heart failure, biokinetics contributes to preserving cardiac reserve, increasing peak VO₂ and alleviating dyspnoea. For stroke recovery, it aids neuroplasticity, restores mobility and improves coordination. Without biokinetics, patients may face greater reliance on medication, diminished long-term control, higher hospitalisation rates and increased risks of complications such as recurrent stroke, muscle atrophy and reduced quality of life.
Metabolic and Endocrine Disorders
Conditions like type 2 diabetes mellitus, metabolic syndrome, dyslipidaemias, obesity and polycystic ovary syndrome rely on medications such as metformin, insulin, statins and hormonal therapies to regulate blood glucose, insulin sensitivity and lipid levels. Biokinetics enhances these outcomes by improving glucose uptake, lowering HbA1c levels, supporting sustainable weight reduction and promoting favourable lipid profiles, including increased HDL cholesterol.
Its inclusion in care plans is vital for addressing all components of metabolic syndrome in parallel and improving endothelial function. Without biokinetics, patients may struggle with poor glycaemic control, rising insulin resistance, heavier medication reliance, worsening syndrome markers and sustained cardiometabolic risk.
Respiratory Diseases
Chronic respiratory conditions, including COPD, asthma, interstitial lung disease, cystic fibrosis and post-COVID-19 syndrome, are primarily managed with bronchodilators, corticosteroids and symptom-specific treatments. These medications work to reduce inflammation, dilate the airways and control fatigue and breathlessness.
Biokinetics reinforces treatment goals by increasing exercise tolerance, improving oxygen use, restoring functional capacity and aiding respiratory recovery. Without it, patients may face worsening dyspnoea, progressive physical deconditioning, more frequent symptoms and greater reliance on relief medications.
Neurological and Neurodegenerative Conditions
In conditions such as Parkinson’s disease, multiple sclerosis, peripheral neuropathies, traumatic brain injury, epilepsy and Alzheimer’s disease, pharmaceutical approaches help manage motor dysfunction, reduce inflammation or prevent seizures. Biokinetics, however, plays an indispensable role in restoring motor function, improving gait and strength, enhancing coordination and supporting neuroplasticity.
Without biokinetics, recovery may be delayed and patients may face accelerated functional decline, increased fall risk and long-term disability. For vestibular disorders, biokinetics contributes by improving balance and reflex compensation; its absence often results in chronic imbalance, movement avoidance and social isolation.
Cancer and Oncology Rehabilitation
Patients with cancers such as breast, colorectal, lung, prostate, haematologic and gynaecologic types, as well as paediatric cancer survivors, typically undergo chemotherapy, immunotherapy and hormone therapy. While these treatments combat disease progression, they can also lead to fatigue, muscle loss and weakened immunity.
Biokinetics alleviates these effects by preserving muscular strength, improving everyday functioning, supporting immune system recovery and helping with postural and mobility adaptations. In its absence, cancer survivors may experience prolonged fatigue, impaired resilience, reduced mobility and, for children, delays in physical development and reintegration.
Paediatric and Developmental Disorders
Paediatric conditions such as cerebral palsy, childhood obesity, autism spectrum disorder, ADHD and juvenile idiopathic arthritis are often addressed through medication targeting symptoms like spasticity, anxiety or inflammation. Biokinetics plays a central role in improving mobility, refining motor skills, supporting behavioural regulation and encouraging physical engagement.
Without biokinetics, children are more likely to experience persistent hyperactivity, diminished coordination, progressive joint deformities and developmental delays. In conditions like congenital heart disease and muscular dystrophies, it helps ensure safe activity, delay muscular decline and reduce the risk of long-term dependence and psychosocial distress.
Referral Pathways Chronic Disease Management
Biokinetics is integrated into the healthcare system through both referral-based and direct-access models. The direction of care, level of coordination, point of entry and expected outcomes are all shaped by how patients enter the system and the role of the referring physician in the broader management of chronic disease.
1. Referral-Based Biokinetics Treatment
When a patient is referred by an allied health professional or specialist, their condition is usually already clinically established, often supported by diagnostic imaging, laboratory results or a documented history of chronic medication use. In these cases, the biokineticist adheres to the referrer’s diagnosis and clinical insights and embarks on condition-specific exercise programming. This interprofessional care model ensures alignment of goals, shared accountability and continuity of care. All interventions are thoroughly documented, with ongoing communication maintained between the biokineticist and the referring practitioner.
Biokineticists play a critical role in managing chronic conditions and optimising function following diagnosis, working under the referral of a health or medical practitioner, as outlined in the scope of practice by the Health Professions Council of South Africa. Table 2 illustrates how interdisciplinary and multidisciplinary collaborations are implemented in clinical practice.

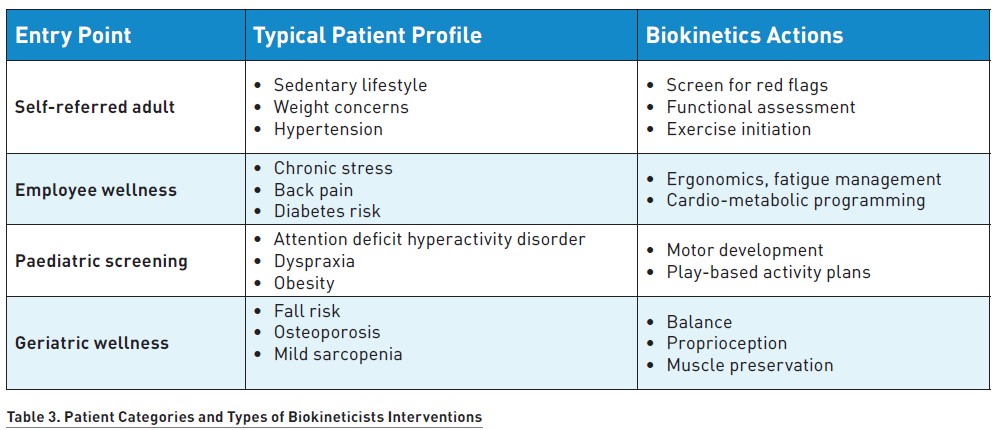
2. Direct Access / Self-Referred Biokinetics Treatment
Biokineticists also work with unreferred patients, particularly at the prevention, wellness or early symptomatic stages, as illustrated in Table 3. These individuals may present with non-specific symptoms such as weight gain, fatigue or mild postural pain, or they may be proactively managing chronic disease risk factors through lifestyle interventions.
In such cases, biokineticists perform risk stratification and a functional baseline assessment. If any clinical red flags or signs of undiagnosed pathology are identified, the patient is referred to a medical doctor prior to initiating the planned intervention.
Regardless of the referral pathway, biokinetics practice is grounded in long-term disease rehabilitation principles. These include:
- individualised exercise prescription guided by scientific standards,
- application of progressive overload and adaptation tailored to medical stability,
- consistent interdisciplinary communication, collaboration and documentation,
- outcome measurement across domains such as pain, strength, balance, quality of life and functional capacity in daily activities.
Interdisciplinary Collaboration in Chronic Disease Management
Biokinetics is most effective when integrated into multidisciplinary and interdisciplinary care teams, working in synergy with other healthcare professionals to maximise patient outcomes. Key contributors to chronic disease management include:
- Physicians (General Practitioners and specialists): responsible for diagnosis, prescribing treatments and providing ongoing medical monitoring;
- Nurses: play a vital role in patient education, medication administration and symptom monitoring;
- Dietitians: develop personalised nutritional plans that support disease management, often integrating dietary changes with physical activity;
- Physiotherapists: focus on manual therapy, movement correction and acute rehabilitation, while biokineticists extend this work by enhancing functional capacity through structured exercise;
- Psychologists: address mental and behavioural health concerns and often work alongside biokineticists, using exercise as a tool to support psychological well-being.
Interprofessional care in chronic disease management ensures that everything that regards the patient's well-being is taken into consideration, from lifestyle change to pharmaceutical optimisation, leading to a better and longer-lasting process of healing.
Conclusion
Biokinetics has become an essential part of chronic disease management worldwide. It stands as a patient-centred, evidence-based treatment that optimises functional capacity, decreases readmission and enhances quality of life for chronically ill persons.
Since the chronic disease burden will continue increasing across the world, multidisciplinary treatment involving biokinetics offers an effective means of improving clinical outcomes and reducing the long-term economic impact of NCDs. Integrating exercise therapy into medical care enables health systems to adopt more holistic and inclusive approaches that address the diverse needs of patients.
Biokineticists, working alongside other healthcare professionals, help maximising patient rehabilitation and restoring functional autonomy, ultimately contributing to healthier and more resilient populations worldwide. Biokinetics' role as an indispensable adjunct to chronic disease care has just begun to be acknowledged broadly. With continued research, professional training and integration into health systems, biokinetics is set to remain a vital contributor to improved patient outcomes and enhanced quality of life around the world.
Conflict of Interest
None.
References:
American College of Sports Medicine (ACSM) (2018) ACSM's Guidelines for Exercise Testing and Prescription. 10th ed. Philadelphia: Wolters Kluwer Health.
American Diabetes Association (ADA) (2014) Standards of Medical Care in Diabetes—2014. Diabetes Care, 37(1):14–80.
Buchheit M & Laursen PB (2013) High-Intensity Interval Training: Solutions to the Programming Puzzle. Sports Medicine, 43(5):313–338.
Carter J & Pritchard J (2017) Chronic Disease Management: The Role of Physical Activity and Exercise. Journal of Chronic Disease Management, 12(2):117–123.
Health Professions Council of South Africa (HPCSA) (2020) Biokinetics Scope of Practice. (accessed: 21 June 2025). Available from hpcsa.co.za
Health Professions Council of South Africa (HPCSA) 2016. Regulations Relating to the Registration of Biokineticists and the Scope of Practice of Biokinetics in South Africa (accessed: 21 June 2025). Available from hpcsa.co.za
Khaw K-T, Wareham N, Bingham S et al. (2008) Physical Activity and Mortality in the European Prospective Investigation into Cancer and Nutrition (EPIC) Norfolk Study. British Medical Journal, 337:a501.
Krebs P, Prochaska JJ & Rossi JS (2010) A Meta-Analysis of Computer-Tailored Interventions for Health Behavior Change. Preventive Medicine, 51(3–4):214–221.
Norris SL, Zhang X, Avenell A et al. (2005) The Effectiveness of Exercise in the Prevention and Management of Type 2 Diabetes Mellitus. Diabetes Care, 28(6):1628–1637.
Sallis JF & Owen N (2015) Ecological Models of Health Behavior. In: K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health Behavior and Health Education: Theory, Research, and Practice (pp. 43–64). San Francisco: Jossey-Bass.
World Health Organization (WHO) (2014) Global Status Report on Noncommunicable Diseases 2014. Geneva: World Health Organization.
World Health Organization (WHO) (2020) Noncommunicable Diseases. (accessed: 21 June 2025). Available from who.int/news-room/fact-sheets/detail/noncommunicable-diseases