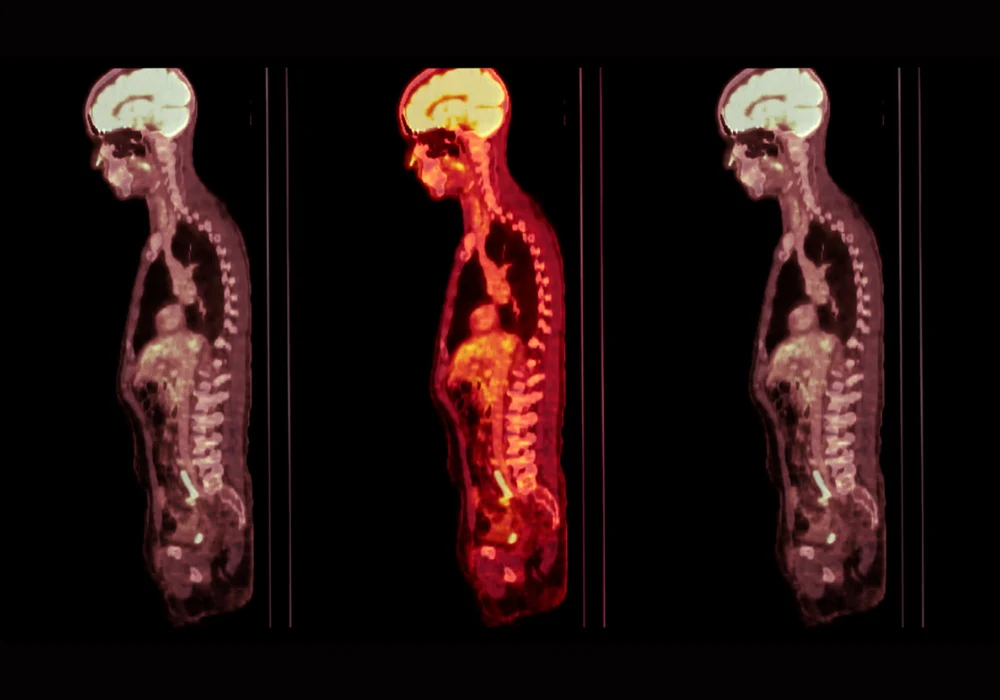
Total-body PET, also known as long–axial-field-of-view (LAFOV) PET, offers significantly enhanced imaging capabilities through increased sensitivity, reduced radiopharmaceutical dose and shorter scan durations. Despite these benefits, the technology’s high capital and operational costs present a barrier to widespread adoption. In Australia, a novel shared model between the Royal North Shore Hospital and the University of Sydney has demonstrated how such technology can be successfully integrated into a dual clinical and research setting. This joint venture addresses funding, governance, staffing and technical challenges while ensuring optimal utilisation of a high-value imaging resource.
A Strategic Partnership for Shared Access
The establishment of the LAFOV PET/CT system at Royal North Shore Hospital was enabled by funding from the Australian government's National Imaging Facility, part of the National Collaborative Research Infrastructure Strategy. Recognising the challenges of limited academic throughput, the University of Sydney partnered with a clinical facility to ensure full utilisation. A formal Memorandum of Understanding defined the terms of ownership, cost-sharing and operational responsibilities for the ten-year agreement. Under this model, hospital use is prioritised during morning hours, performing 16–20 clinical scans daily, with afternoons reserved for research activities.
The PET/CT system replaced an older unit without altering staffing levels or increasing costs. Hospital staff operate the scanner at all times, meeting regulatory standards and reducing expenses for the university. The collaboration has also yielded efficiency gains, such as the reduced use of radiopharmaceuticals, which are charged by activity in Australia. Clinical scan duration was standardised to five minutes using 120–150 MBq, leading to a 40% reduction in the hospital’s annual PET radiopharmaceutical budget without sacrificing image quality.
Operational Efficiency and Technical Adaptation
Selecting a Biograph Vision Quadra system with a 106 cm axial field of view allowed for whole-body imaging in a single scan position. Following installation, rigorous testing was conducted using a range of radiopharmaceuticals to optimise acquisition parameters. Scheduled at 15-minute intervals, the system supports a relaxed clinical pace but could accommodate shorter intervals if necessary.
Must Read: Enhancing 82Rb PET/CT Image Quality with Positron Range Correction
To manage the complexity of dual use, the Memorandum of Understanding included provisions for flexibility in scheduling, recognising the time-sensitive nature of radiopharmaceuticals and patient conditions. Dedicated DICOM nodes were established to ensure separation of hospital and research data, supporting privacy and compliance standards.
Ethical and procedural governance was also carefully structured. For research scans, incidental findings are not routinely reviewed by clinicians. If abnormalities are noticed during quality checks, escalation follows predefined protocols managed by the principal investigator. This separation of responsibilities respects the different regulatory environments of clinical care and academic research.
Scientific Collaboration and Clinical Benefit
Beyond resource sharing, the joint facility has created new opportunities for innovation. University researchers developed protocols for dynamic whole-body scans by injecting patients directly on the scanner bed and extending the scan duration to 50 minutes. This method, conducted during routine scans, does not disrupt clinical workflows and allows researchers to access data without incurring additional costs.
To support such research, a low-dose CT protocol was implemented using a tin filter and reduced beam settings, yielding an effective dose below 0.5 mSv. Although not ideal for clinical diagnosis due to lower image clarity, these scans provide accurate PET attenuation corrections and have been adopted for specific patient groups. In clinical practice, the protocol has proven especially valuable for scanning young or pregnant patients, significantly reducing radiation exposure without compromising diagnostic accuracy.
This mutual reinforcement between research and clinical practice illustrates the model’s adaptability. While researchers benefit from access to high-quality imaging data, clinicians gain from advanced protocols developed through collaborative experimentation. The ability to safely perform scans with minimal radiation has enhanced the hospital’s diagnostic capabilities, especially for vulnerable populations.
Eighteen months into operation, the shared LAFOV PET/CT facility has met both clinical and research demands with efficiency and flexibility. The model has allowed the hospital to scan more patients in less time while reducing staff radiation exposure and radiopharmaceutical costs. Although clinical scheduling is limited to half-days, the trade-off in capital and operational savings is substantial.
The success of this initiative demonstrates how academic and clinical institutions can overcome the financial and logistical barriers of cutting-edge imaging infrastructure through strategic collaboration. The Royal North Shore Hospital and University of Sydney’s joint model provides a scalable framework for other centres seeking to deploy LAFOV PET systems. With improved patient experience, high image quality and reduced resource usage, this integrated approach aligns both scientific discovery and clinical excellence.
Source: The Journal of Nuclear Medicine
Image Credit: iStock