A new technique for cardiac magnetic resonance (CMR) imaging can improve accuracy by removing patients’ need to breathe, as the lack of motion allows acquisition of higher quality images in less time, according to research presented at EuroCMR 2016 in Florence, Italy.
“In many imaging techniques, but particularly in CMR, you need a relatively long acquisition time and must correct for respiratory motion,” said Professor Juerg Schwitter, director of the Cardiac MR Centre at the University Hospital Lausanne, Switzerland.
“For decades we have had to correct for respiration when estimating the position and motion of the heart by CMR, and this is not always accurate,” he told the meeting organised by the European Association of Cardiovascular Imaging (EACVI) in collaboration with the Society for Cardiovascular Magnetic Resonance, the Asian Society for Cardiac Imaging, the European Society for Cardiac Radiology and other associations and working groups of the European Society of Cardiology.
“In Lausanne, radio-oncologists are exploring a technique called high frequency percussive ventilation,” Prof. Schwitter continued.
“Patients do not need to breathe naturally and no correction for respiratory motion is required. This enables the physicians to more accurately plan the field of radiation to apply in each patient.”
For the technique, patients put a mask over their mouth which is connected to a ventilator that delivers small volumes of air, called “percussions.” Instead of the 10 to 15 large breaths patients would take naturally per minute, air is provided in 300 to 500 small ventilations per minute. Air volumes are small so the chest does not move. The procedure is noninvasive, patients are conscious, not sedated, and do not need to breathe.
For the current study, the ventilator was adapted for use in the CMR environment. CMR uses a magnet which means that metal parts had to be swapped for MR-compatible ones. Tubes were used to connect equipment inside and outside the scanning room.
Professor Schwitter said: “Patients lie face up in the CMR machine and do not need to breathe. They say their chest feels a bit inflated during the ventilation but otherwise it feels okay.”
The study was designed to test the feasibility and tolerability of high frequency percussive ventilation during CMR. It included one healthy volunteer aged 38 years and one patient aged 55 years with a thymic lesion. The procedure was well tolerated in both cases. The average time without breathing was ten minutes in the volunteer and six minutes in the patient.
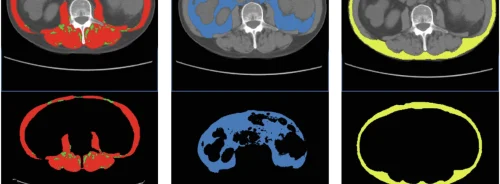
The investigators could clearly see the coronary arteries. Lung volumes were “frozen” in full inspiration and the pulmonary vessels were also seen clearly. There was no need to correct for respiratory motion.
Prof. Schwitter added: “We found that this type of ventilation was feasible and there was no problem with tolerating it. Of course, we are in a very early stage of development and we now need to test it in more patients. Some patients may find it difficult because the CMR machine is small and on top of that they will be ventilated by a machine.”
CMR images are currently acquired in steps. Patients breathe in and then hold their breath for each image, then recover before repeating the process for the next image. High frequency percussive ventilation offers the potential to acquire all images in one go, with no need to correct for respiratory motion.
“The possibilities with high frequency percussive ventilation are huge,” said Prof. Schwitter. “You could run all the CMR sequences in one batch, which would be much faster. Data could be acquired constantly with fewer artifacts. We might be able to use this technique for diagnosis of sicker patients, who find breath holding difficult and need the imaging to be done quickly.”
“This technique would help us to collect high resolution images where we want millimetric precision, for example to localise scar in the myocardium or to see the anatomy of coronary arteries or valves and malformations. We would have much better conditions because we would not need to correct for motion.”
Prof. Schwitter concluded: “In future, we could even imagine that if the patient is not breathing for 20 minutes or even longer this technique could give a precise 3D representation of cardiac structures and help guide electrophysiology procedures, such as ablation.”