Over the past decade, MRI-targeted biopsy has emerged as a superior method for detecting clinically significant prostate cancer (csPCa) compared to systematic biopsy. Randomized studies have consistently demonstrated its efficacy. However, MRI fails to detect up to one-third of csPCa cases. This shortfall is influenced by histopathologic features such as Gleason grade, tumour volume, and cellular density, which affect the visibility of prostate cancer on MRI. Additionally, certain histologic subtypes, like mucinous adenocarcinoma, are less conspicuous on MRI. Intraductal carcinoma (IDC) and invasive cribriform (Cr) subtypes are associated with increased aggressiveness and adverse clinical outcomes. Yet, their detectability via MRI remains controversial, prompting further investigation into the capabilities of MRI-targeted biopsy in identifying these aggressive subtypes.
MRI-Targeted Biopsy: Superior Detection of Clinically Significant Prostate Cancer
MRI-targeted biopsy has been proven superior in detecting clinically significant prostate cancer (csPCa) compared to systematic biopsy. This method involves using multiparametric MRI (mpMRI) to identify suspicious areas, which are then targeted for biopsy. Several studies have confirmed the efficacy of MRI-targeted biopsy. For instance, research has shown that MRI can detect 77% of csPCa found at radical prostatectomy. The MRI-targeted approach reduces the risk of overdiagnosis by half, avoiding unnecessary treatments and focusing on significant lesions.
Furthermore, MRI-targeted biopsy has shown a higher detection rate of aggressive cancer types. The advantage lies in the ability of MRI to provide detailed imaging that highlights potential cancerous areas, allowing for precise targeting during biopsy. This targeted approach contrasts with systematic biopsy, which samples the prostate at regular intervals and often misses significant lesions. Given its higher accuracy, MRI-targeted biopsy is increasingly preferred for diagnosis, risk stratification, and monitoring of prostate cancer, effectively replacing systematic biopsy in many clinical settings.
Challenges in Detecting Cribriform and Intraductal Carcinoma Subtypes
Despite the overall success of MRI-targeted biopsies, detecting IDC and Cr subtypes remains challenging. IDC and Cr subtypes are known for their aggressiveness and poor prognostic implications. These subtypes are linked with increased genomic instability, higher rates of biochemical relapse, and a greater likelihood of distant metastases. Consequently, their detection is crucial for accurate prognosis and treatment planning.
The sensitivity of MRI for detecting Cr/IDC-pattern prostate cancer varies widely, with reports ranging from 17% to 96%. This wide range indicates inconsistencies in detection, which could be attributed to the variability in MRI techniques, interpretation, and the intrinsic characteristics of the tumours. IDC and Cr subtypes often coexist and are difficult to distinguish on conventional haematoxylin and eosin-stained slides, requiring specific reporting by pathologists. These subtypes significantly impact prognostic assessments and treatment decisions, including exclusion from active surveillance and minimally invasive focal therapies. Improved detection methods are necessary to identify these aggressive subtypes and enhance patient outcomes reliably.
Comparing MRI-Targeted and Systematic Biopsy for Cr/IDC Detection
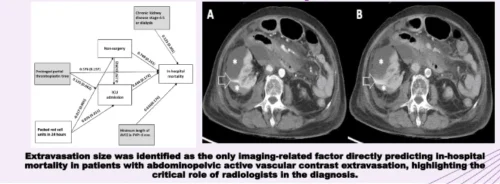
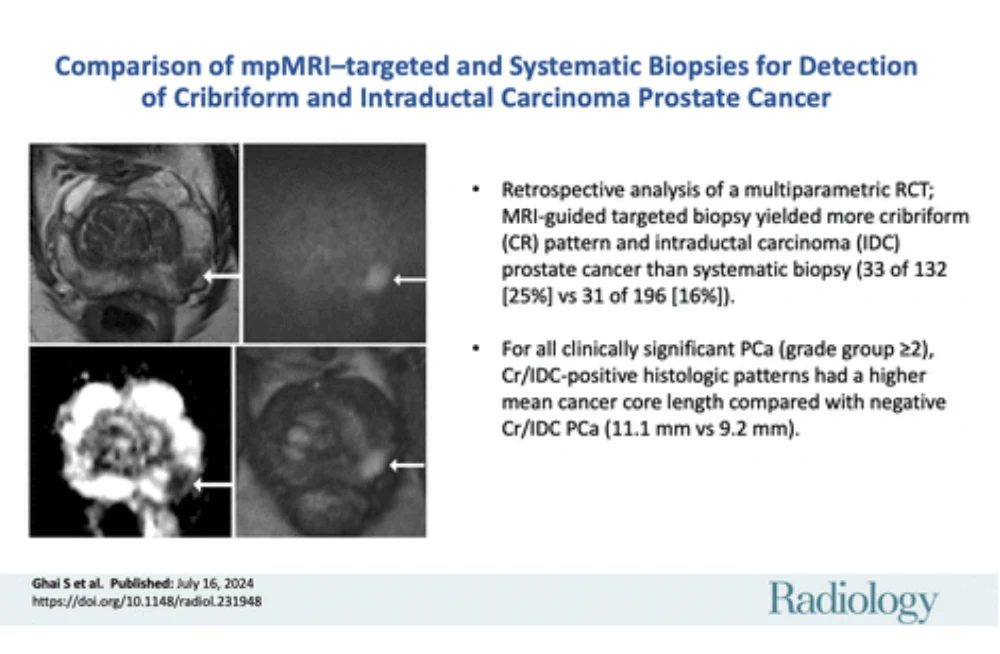
A phase 3 multicentre randomised controlled trial aimed to compare the detection rates of Cr/IDC subtypes in biopsy-naive men undergoing either MRI-targeted or systematic biopsy. The trial included 453 participants with a clinical suspicion of prostate cancer. Participants were randomised to undergo either systematic 12-core biopsy or MRI-targeted biopsy. Only those with a Prostate Imaging Reporting and Data System (PI-RADS) score of 3 or higher underwent biopsy in the MRI arm.
The study revealed a higher detection rate of Cr/IDC patterns in the MRI-targeted biopsy group (25%) compared to the systematic biopsy group (16%). Specifically, Cr/IDC prostate cancer was detected in 33 out of 132 participants in the MRI-targeted biopsy arm and 31 out of 196 participants in the systematic biopsy arm. This higher detection rate underscores the effectiveness of MRI-targeted biopsy in identifying aggressive cancer subtypes.
Moreover, among participants with negative findings for Cr/IDC at initial biopsy, those in the MRI-targeted biopsy arm were numerically less likely to have Cr/IDC csPCa detected on prostatectomy specimens compared to those in the systematic biopsy arm (24% vs. 69%). Although the results did not reach statistical significance, this trend suggests that MRI-targeted biopsy provides a more accurate assessment of aggressive histologic patterns, which is crucial for pretreatment risk stratification and clinical decision-making.
MRI-targeted biopsy has demonstrated superior efficacy in detecting clinically significant prostate cancer, particularly aggressive subtypes like cribriform and intraductal carcinoma, compared to systematic biopsy. While challenges remain in consistently identifying these subtypes, MRI-targeted biopsy represents a significant advancement in prostate cancer diagnostics. The higher detection rates of Cr/IDC patterns in MRI-targeted biopsies highlight the importance of incorporating this method into clinical practice.
Further research and technological advancements are necessary to enhance the accuracy and reliability of MRI in detecting all prostate cancer subtypes. This includes improving MRI techniques, standardising interpretation criteria, and exploring the potential of combining MRI with other diagnostic modalities. Ultimately, integrating MRI-targeted biopsy into routine clinical practice could lead to better patient management, more accurate risk stratification, and improved clinical outcomes by providing a more precise and comprehensive diagnostic tool for prostate cancer.
Source & Image Credit: Radiology