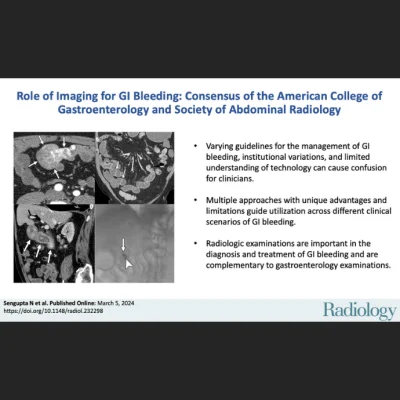
Gastrointestinal (GI) bleeding is a common cause of hospitalization, requiring prompt diagnosis and treatment to improve patient outcomes and reduce healthcare costs. Various radiologic techniques, such as CT angiography, catheter angiography, CT enterography, MR enterography, nuclear medicine red blood cell scan, and technetium-99m pertechnetate scintigraphy (Meckel scan), are used alongside GI endoscopy to evaluate GI bleeding. However, guidelines on their usage vary, leading to confusion among clinicians. A joint effort by the American College of Gastroenterology and Society of Abdominal Radiology offers consensus recommendations on the utilization of these radiologic examinations, aiming to enhance understanding and standardise practices in assessing GI bleeding. A comparison of advantages and limitations relative to endoscopic examinations was published in Radiology, and the recommendations on roles and indications are reproduced below.
Recommendations for Imaging in Overt LGIB
CT Angiography
Technique.
- Unenhanced images (conventional or virtual non-contrast) should be acquired in all cases.
- Images should be acquired during a late arterial phase and a portal venous or delayed phase.
- No oral contrast material should be administered.
- Three-dimensional CTA images can be generated to help guide subsequent conventional angiography.
- Dual-energy CT techniques may be used if available to improve the visibility of sites of contrast material extravasation.
Role/indications.
- CTA should be performed as the first diagnostic study in hemodynamically unstable patients.
- CTA could be considered as the first-line study in hemodynamically stable patients where the suspicion of active bleeding is high.
- CTA is not indicated as a first-line test in hemodynamically stable patients in whom bleeding has subsided.
Catheter Angiography
Technique.
- CA for LGIB can be performed through common femoral artery or radial artery access.
- Permanent agents, such as micro coils or glue, are used to embolize the vasa recta at the site of identified bleeding.
- In the absence of active extravasation at angiography, embolization should not be performed, as the exact site of bleeding is not identified.
Role/indications.
- In most cases, if CTA is negative for GI bleeding, CA is not indicated.
- In unstable patients with active extravasation at CTA, CA with embolization can be used as the primary treatment modality.
- If the patient has recurrent intermittent LGIB and all modalities have failed to identify the source of bleeding, provocative CA can be performed to identify and treat the culprit lesion.
99mTc-RBC Scan Nuclear Medicine
Technique.
- The in vitro RBC labelling method has the highest labelling efficiency and is the preferred method.
- Imaging should be continued for 1 hour if no bleeding is detected.
Role/indication.
- In a hemodynamically stable patient with evidence of ongoing LGIB, negative evaluation with colonoscopy, and a CTA examination is negative, contraindicated, or not available, tagged RBC scanning can be performed.
Recommendations for Imaging in Suspected Small Bowel Bleeding
CT Enterography
Technique.
- CTE should be performed using multiphase technique in patients older than 40 years of age where vascular lesions are a common cause for bleeding.
- Multiphase CTE should include at least arterial, and enteric or portal venous phases.
- Multiphase CTE is the recommended term for a CTE examination performed for suspected small bowel bleeding and acquired with multiple phases after the administration of intravenous contrast material.
- A single phase performed during the enteric or portal venous phase is adequate to evaluate for inflammatory conditions such as Crohn disease, radiation enteritis, nonsteroidal anti-inflammatory drug enteropathy, and most malignancies.
- Neutral enteric contrast material should be administered in divided doses beginning 1 hour before CTE.
Role/indications.
- CTE should be performed instead of CTA in hemodynamically stable patients presenting with ongoing suspected small bowel bleeding after negative colonoscopy and esophagogastroduodenoscopy (EGD) and capsule endoscopy (if negative or not performed).
- If there is brisk ongoing bleeding with hemodynamic instability, CTA should be performed instead of CTE.
- CTE should be the first-line imaging test for suspected small bowel bleeding in hemodynamically stable patients if patients are at increased risk for video capsule retention.
- CTE should be the first-line study for suspected small bowel bleeding in hemodynamically stable patients if small bowel neoplasm is the suspected cause for small bowel bleeding.
- CTE can be performed as the first-line diagnostic study for suspected small bowel bleeding in hemodynamically stable patients depending on clinical scenarios such as local availability and expertise.
- CTE should be performed if there is no definitive cause for small bowel bleeding identified at capsule endoscopy and there is suspicion for ongoing bleeding.
Meckel Scan
Role/indication.
- A Meckel scan can be considered to identify the cause of unexplained intermittent GI bleeding in children and adolescents after negative endoscopic evaluation, including capsule endoscopy if available, and cross-sectional evaluation of the small bowel.
Recommendations for Imaging in Nonvariceal UGIB
Catheter Angiography
- CA with intent to treat is indicated when an EGD is unsuccessful in achieving initial hemostasis, or the patient experiences recurrent bleeding after a successful initial EGD and a repeat EGD is either unsuccessful or not recommended.
CT Angiography
- In the setting of ongoing bleeding, CTA can be considered:
- If the patient is not thought to be suitable for EGD or if there is no in-house emergency gastroenterology coverage.
- After negative EGD or if EGD is unable to identify the site of bleeding.
Source & Image Credit: Society of Abdominal Radiology and the American College of Gastroenterology