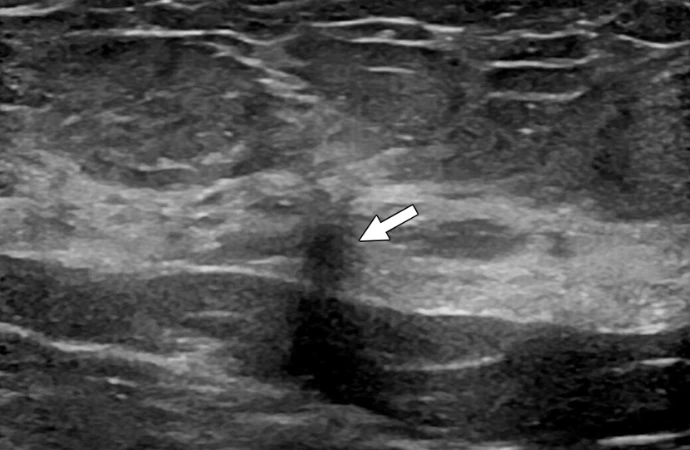
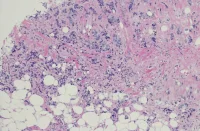
Radial scars are abnormal growths in the breast tissue with a characteristic appearance on histopathology. They are increasingly being detected due to improved imaging techniques. Historically, they were often surgically removed due to concerns about potential cancer risk, but recent studies show variable rates of cancer upstaging following surgery. However, these studies have limitations, including the mix of different types of radial scars and the reliance on older imaging technology. This study published in the American Journal of Roentgenology aims to determine the risk of cancer upstaging in radial scars detected through modern imaging methods and identify factors that may indicate a higher cancer risk.
Insights from Combined Digital Breast Tomosynthesis and Mammography
This retrospective study, conducted at a single academic medical centre, aimed to assess the upstaging rates of radial scars detected through combined digital breast tomosynthesis (DBT) and digital mammography (DM) and to identify factors associated with upstaging risk. The study analysed data from patients who underwent core needle biopsy (CNB) for radial scars between January 2013 and December 2020. A total of 49 patients were included, meeting specific criteria, such as undergoing surgical excision or a minimum of 2 years of imaging surveillance post-CNB. Data on patient demographics, imaging findings, biopsy procedures, and histopathology were collected from electronic medical records (EMR). Histopathology slides from CNB and surgical excision were reviewed for classification and presence of atypia. Statistical analysis, including descriptive summaries and logistic regression, was performed to assess upstaging rates and identify predictive factors. The study utilised R statistical software for analysis.
Predictors of Cancer Upstaging in Radial Scars Detected via Screening DBT and DM
The study initially identified 165 women with 171 radial scars detected through screening DBT and DM, excluding 12 patients who didn't undergo surgical excision or follow-up imaging. The final sample included 153 women with 159 radial scars, mostly white and aged around 56. Biopsy reports classified most lesions as radial scars, with some termed complex sclerosing lesions. A significant portion of patients had a prior breast cancer diagnosis or a family history of breast cancer. Mammographic findings varied, with architectural distortion being the most common. Most radial scars underwent mammographically guided biopsy. About 19% of radial scars had associated atypia at CNB.
Of the 159 radial scars, 80.5% underwent surgical excision, with 7.8% being upstaged to cancer. Among radial scars with atypia, the upstaging rate was 20.0%, significantly higher than those without atypia. Upstaging risk was associated with older age, a history of breast cancer, and the presence of atypia at CNB. Notably, radial scars presenting as calcifications had a lower upstaging rate.
In summary, the study found that older age, a history of breast cancer, and the presence of atypia at CNB were significant predictors of upstaging to cancer in radial scars detected through screening DBT and DM.
Management Considerations & Limitations for Radial Scars Detected via Screening DBT
In a study involving 153 women with 159 radial scars identified through screening DBT, 5.0% of radial scars were upstaged to cancer, with a significantly higher upstaging rate observed in radial scars with atypia compared to those without (20.0% vs. 1.6%). Notably, none of the radial scars presenting as calcifications were upstaged to cancer, suggesting that surveillance may be a reasonable management strategy for such cases, especially when no atypia is present.
Current guidelines lack consistency regarding the management of radial scars, with some advocating for surgical excision while others support surveillance. The study's findings align with recent research indicating low upstaging rates for radial scars without atypia detected through DBT and DM, suggesting that surveillance may be warranted instead of surgical excision, irrespective of sonographic lesion size or biopsy guidance modality.
However, it's essential to note that even radial scars without atypia may show atypia upon surgical excision, emphasising the importance of surgical consultation to discuss the potential discovery of high-risk pathology and the option for excision versus surveillance.
Factors associated with upstaging risk besides atypia include older age, a prior breast cancer diagnosis, and a family history of breast cancer. These findings can help inform clinical management decisions regarding surgical excision versus surveillance.
While the study sheds light on the management of radial scars, it has limitations, including its retrospective nature, the lack of uniform imaging protocols for surveillance, and the focus on asymptomatic individuals with DBT-detected radial scars, potentially limiting generalizability.
The study supports the notion that radial scars without atypia detected through DBT can be safely followed rather than surgically excised. However, factors such as age, medical history, and family history should be considered in decision-making regarding radial scar management.
Source & Image Credit: American Journal of Roentgenology
IMAGE