Automated reading of chest x-rays (CXR) using computer-aided detection (CAD) is recommended for adults in tuberculosis (TB) screening and triage, yet paediatric use remains unaddressed. Childhood TB presents distinct clinical and radiographic patterns, CXR interpretation is variable, and image acquisition in young children is technically challenging. As CXR is often the only adjunctive test available in primary care, there is a clear need for paediatric-specific CAD that can recognise age-related anatomy, typical TB features and common differentials. Progress depends on building suitable data resources, adapting modelling approaches to children and resolving analytical and implementation issues that affect accuracy, equity and practical use.
Building the Right Datasets and Reference Standards
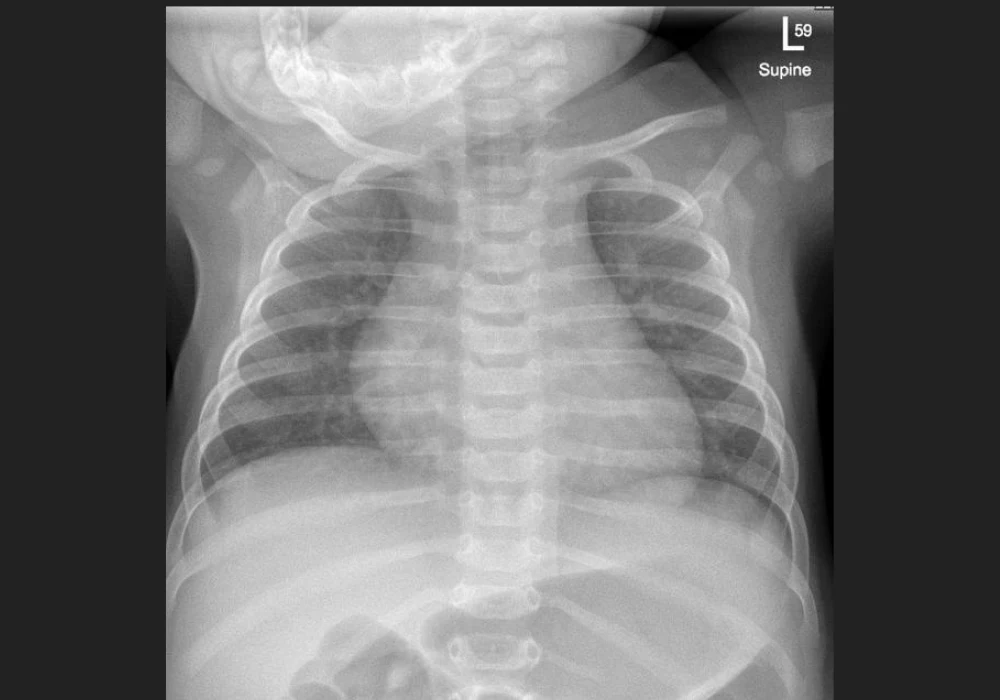
High-quality paediatric repositories are the foundation for effective models. Image sets should prioritise children younger than 10 years, represent diverse geographies and TB burdens and include infants, children living with HIV and those with malnutrition. They should capture the breadth of pathology relevant to TB—such as hilar lymphadenopathy, consolidation, airway compression, pleural effusion and cavitation—alongside non-TB conditions and normal developmental variation, including the presence or absence of the thymus. Variation in hardware, acquisition techniques and image quality is important to reflect real-world practice and reduce bias against underserved populations. Lateral-view CXRs, valuable for assessing hilar lymphadenopathy, should be included even though most commercial systems are not currently trained in this view.
Recommended Read: DL Outperforms Radiomics in Chest X-Ray Classification
Standardised expert labelling is essential. Images should be classified as normal or abnormal, then as consistent or not with TB, using uniform criteria that identify key features and severity indicators. A minimum clinical dataset—age, sex, TB contact history, HIV status and nutritional status—supports subgroup analyses, including infants and differing care settings. Repositories should be matched to intended use, whether asymptomatic screening, differentiation of TB from other respiratory diseases in symptomatic children, or severity stratification to inform regimen choice and duration. Public availability enables transparent development and broader participation in paediatric TB CAD.
Reference standards remain a central challenge. Microbiological confirmation risks excluding many children with paucibacillary disease, whereas clinical standards can embed CXR findings and inflate performance estimates. Using both standards and reporting accuracy consistently against radiographic reads by experts, provides a more balanced assessment. Reporting should align with target product profiles for TB screening, including specificity at fixed sensitivity thresholds.
Model Development and Performance in Children
Most current CAD systems rely on deep learning and large adult datasets, so paediatric models benefit from transfer learning and paediatric-specific preprocessing. Differences in lung size, dose, acquisition parameters and artefacts mean adult-trained preprocessing steps often require adaptation. Studies show that paediatric-focused preprocessing—such as bone suppression fine-tuned on children and robust lung segmentation—improves downstream classification.
Early paediatric CAD efforts for CXR abnormalities achieved moderate accuracy, with weaker performance in basal and perihilar regions that matter for TB. Deep learning models trained for paediatric pneumonia classification demonstrate good discrimination, but many compare diseased with normal images, which can overestimate real-world performance. Evidence specific to TB underscores the gap: a commercial TB CAD model in South African children initially achieved an area under the curve (AUC) of 0.58 for expert-defined TB consistency, improving to 0.72 after fine-tuning on paediatric images, for confirmed versus unlikely TB, AUC improved from 0.68 to 0.78 after fine-tuning. In Gambian children, against a microbiological standard, AUC reached 0.70 with high specificity at the manufacturer threshold but low sensitivity. Adjusting to 90% sensitivity markedly reduced specificity, highlighting the trade-offs and the need for paediatric-appropriate thresholds.
Transfer learning from adult or non-CXR domains and self-supervised approaches can compensate for limited paediatric data and have delivered high accuracy in pneumonia tasks. Multiclass models that distinguish several respiratory conditions show promise for broader clinical utility, though performance often drops in younger children and in cases with reader disagreement, especially around perihilar changes. Given the heterogeneous manifestations of paediatric TB, a single classifier may not detect all disease forms, algorithms that reliably flag abnormal from normal CXRs or identify severe versus non-severe disease, could add clinical value by guiding further testing and treatment decisions.
From Bench to Bedside: Practical Integration
Successful deployment requires more than model accuracy. Expanded access to digital x-ray, technical training and attention to image quality directly affect algorithm performance. Ultra-portable x-ray systems compatible with CAD are promising for low-resource settings but have not been formally assessed in children. The clinical point of use matters, impact may differ between contact screening and facility-based evaluation. Integration into existing paediatric TB decision pathways is necessary to translate outputs into action. Further work should determine whether investment in CAD improves detection and outcomes compared with current or emerging approaches. Even if a dedicated paediatric model proves necessary, validated functionality should be incorporated into existing adult CAD products to support equitable access across age groups.
Child-specific datasets, standardised labelling, appropriate reference standards and paediatric-aware modelling are all required to advance CAD for childhood TB on CXR. Existing evidence shows potential, especially with transfer learning, but performance in children lags behind adult-focused tools and varies by age, anatomy and use case. Collaboration between CAD developers and paediatric TB experts can accelerate development, validation and integration, helping clinicians in constrained settings make faster, better-informed decisions that shorten delays and improve care for children at risk of TB.
Source: The Lancet Digital Health
Image Credit: iStock