The Current Situation and Challenge of COVID-19
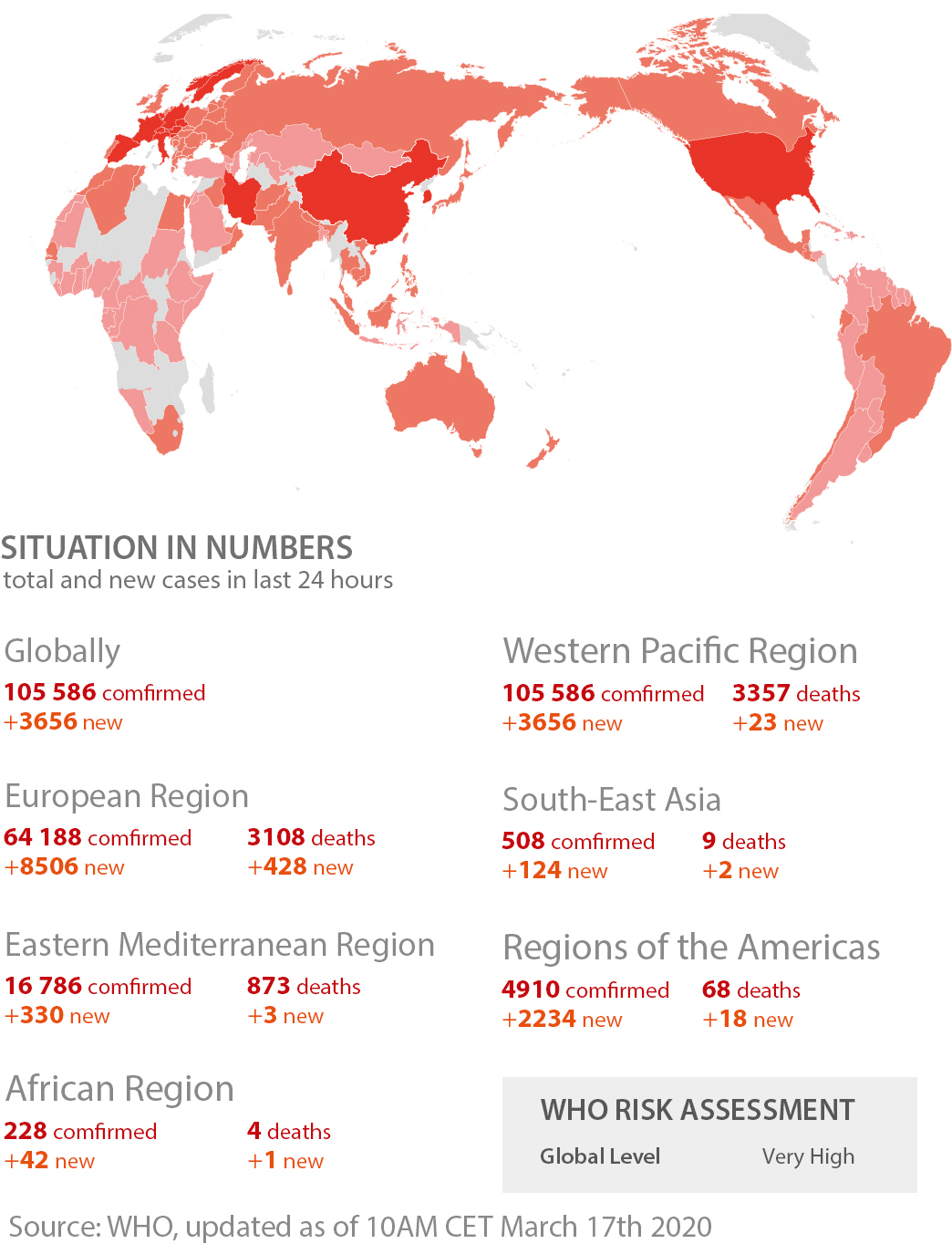

Concensus of Infection Control for Ventilators
1. Infection control during ventilation
- Recommend using single-patient use circuits (water-trap with one-way valve mechanism). Patients with COVID-19 are not adviced to routinely change circuits unless damaged or soiled. Changing circuits leads to the dispersion of contaminated droplets and aerosols, as well as increased use of medical resources (workload and consumables).
- Ventilator circuits have high concentration of pathogens, which may induce VAP. Therefore, condensate should be removed regularly. When disconnecting the ventilator or condensate, avoid accidental splashing of condensate or allowing condensate to go into the patient’s airway. Suggest placing the ventilator on stand-by to suspend the ventilator from operating prior disconnecting the circuits to prevent this.
- Closed-suction is preferred, use suction tube as alterative, and avoid disconnecting the ventilator circuits.
- Place filter in both inspiratory and expiratory end of the ventilator. When using a disposable filter, the exhalation filter requires to be replaced when resistance is increased due to the accumulated condensate increases due to active humidification.
- For invasive ventilation, a heated humidifier (active humidification) with dual heating wires should be used to reduce the formation of condensate in the circuit; or a humidified heat exchanger (passive humidification) with a bacterial filtration function. It is not recommended to add a filter at the Y-tube during active humidification, as it will increase the filter's water content and increase respiratory resistance.
- When using a single-limb non-invasive ventilator, the non-invasive ventilator should use a disposable exhalation valve as much as possible instead of using vented masks. A filter should be added between the mask and the exhalation valve.
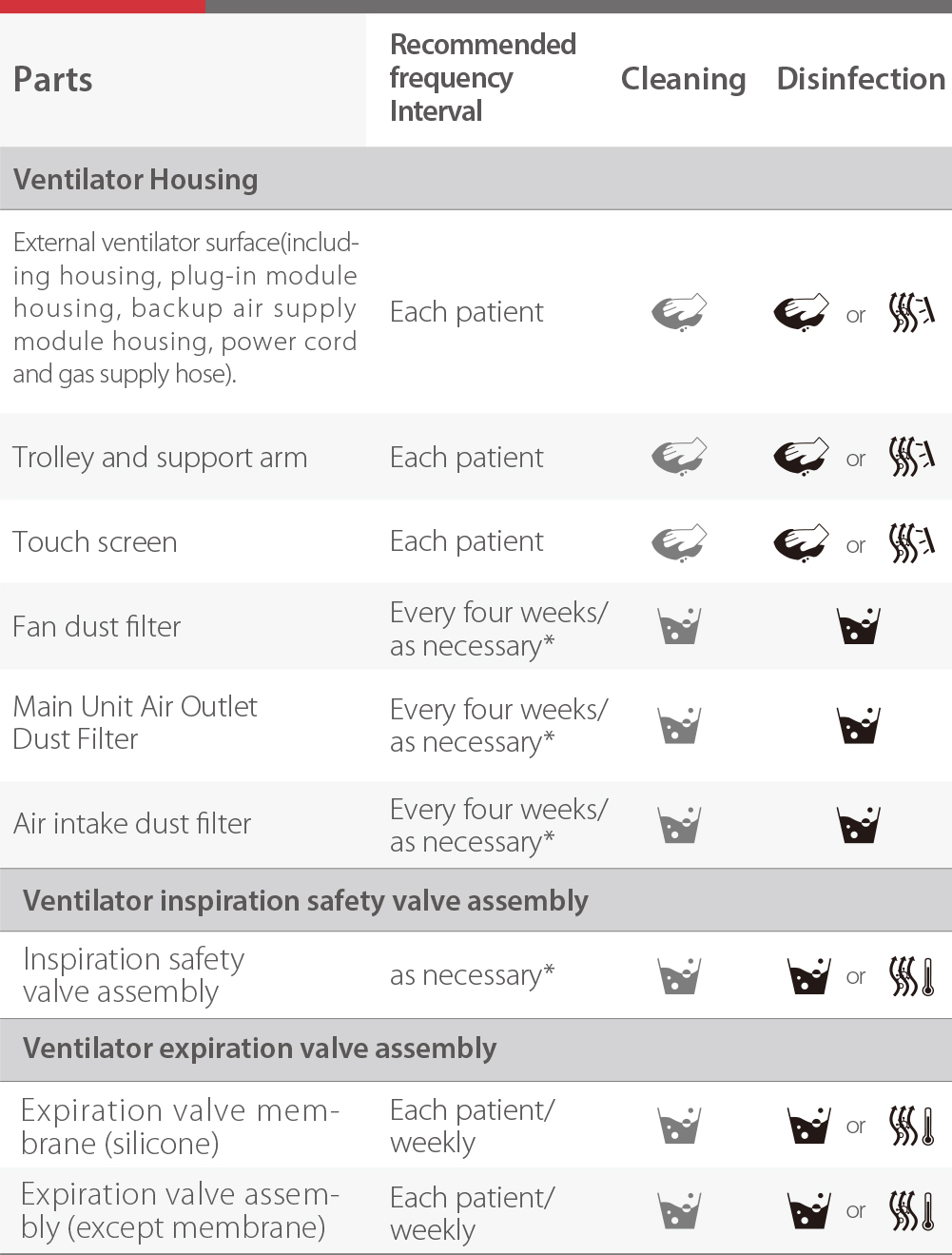
2. Post Ventilator Disinfection
COVID-19 is sensitive to ultraviolet light and heat. 56 C for 30 minutes, ether, 75% ethanol, chlorine-containing disinfectant, and lipid solvents such as peracetic acid and chloroform can effectively inactivate the virus.
- Ventilator surface disinfection: 75% ethanol or hydrogen peroxide to wipe external surfaces (including monitors)
- Handling of breathing circuits: After disposable ventilator circuit is used, it shall be disposed as medical waste. For resusable circuits, disinfection measures should be taken. For the circuits contaminated with COVID-19, it is recommended to use 1:25~1:50 chlorine preparation soak disinfectant (circuits) and high temperature and high pressure (filter) for sterilization.
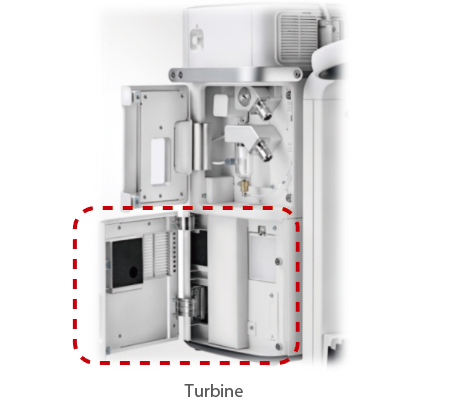
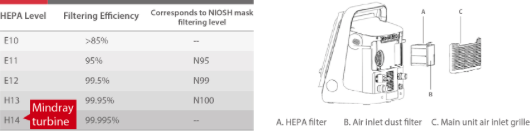
- Ensuring gas sources are clean: Filters are usually installed in central air supply systems. For ventilators that use compressors or turbines to provide high-pressure gas, avoid dust and pathogens in the environment. The ventilator should be equipped with air filters or high-efficiency filters at gas inlet.
- Disinfect inspiratory and expiratory valves: The components of the ventilator that need to be cleaned or disinfected are mainly the flow sensors located in the exhalation valve and in the expiratory side of the ventilator. If a reusable external pressure-differential flow sensor is connected, external sensor should be disinfected together with the exhalation valve. Dispose single-patient use external pressure-differential flow sensors as medical waste.
Infection Control Management for Mechanical Ventilators
Safeguard for Medical Personnel and Patients
3-in-1 device

Avoid aerosol infection
WHO believes that the use of non-invasive positive pressure ventilation (NPPV) with vented mask may be one of the main sources for aerosol transmission in the hospital. The vented mask does not have dedicated filters to process the contaminated gas, so that the gas is directely released to the environment.
Mindray SV ventilators use dual-limb circuit design and non-vented mask for non-invasive ventilation that can highly reduce the amount of aerosol released to the environment during ventilation.

Reliable hardware design: detachable and autoclavable ins-/expiratory valves
The SV Series ventilators are designed according to the latest CE guideline, allowing detachability and autoclavablity for both inspiratory and expiratory valves. The valves can go through steam autoclave at a temperature of up to 134 C. This makes it easier for sterilization and thus prevent the risk of cross-infections. Also, the built-in flow sensor of the expiratory valve can work under high condensation environment and will not be affected by nebulization drugs, making it more stable and reliable. The flow sensor can last for the whole ventilation period without the need of change and hence further the chance of disconnection.

Intergrated with the HEPA Filter
With built-in turbine and backup battery that mean even under the most stringent environment, you patient can still receive ventilation treatment. All the Mindray turbine driven unit come with Level H-14 HEPA filter, this makes it a reliable guardian for both patients and medical personnel.
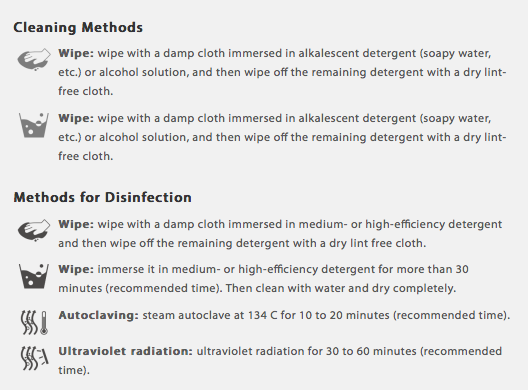
Methods for Cleaning and Disinfection
Reference:
[1] Expert Concensus of Mechanical Ventilation Infection Control for Novel Coronavirus ,Chinese Journal of Respiratory and Critical Care Medicine, Mar. 2020, Vol. 19, No. 2.
[2] WHO: Clinical management of severe acute respiratory infection when Novel coronavirus (2019-nCoV) infection is suspected: Interim Guidance.







