The American Thoracic Society and the Infectious Diseases Society of America have updated guidelines for the diagnosis and management of hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP). A summary of the latest recommendations for practising clinicians is published online in the Annals of the American Thoracic Society.
See Also: Seven Days Antibiotics OK for HAP/ VAP, New Guidelines
"Clinicians should use caution when interpreting the recommendations and should always consider individual clinical circumstances, such as comorbid conditions, local antibiograms, and individual patient values and preferences, when treating patients with hospital-acquired and ventilator-associated pneumonia," the authors note in the journal article.
To help with diagnosis, the updated guideline recommends that cultures of respiratory secretions and blood should be obtained for all patients with suspected HAP/VAP. Regarding the use of biomarkers, including procalcitonin and C-reactive protein, to increase the accuracy of the diagnosis of VAP, the authors write: "On the basis of the current sensitivity and specificity of these biomarkers, clinical criteria alone should be used to initiate antibiotic therapy for suspected HAP/VAP."
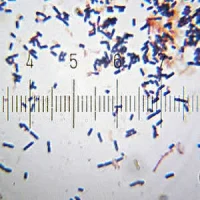
In treating patients with suspected VAP, the guideline recommends including coverage for S. aureus, Pseudomonas aeruginosa, and other gram-negative bacilli in all empiric regimens. In the article, the authors have noted that inadequate initial therapy for VAP is associated with poor outcomes, whereas antibiotic resistance is common. Broad coverage of commonly isolated pathogens and resistance patterns is recommended, according to the article, although prospective trials have not compared regimens with and without agents active against one or more potentially resistant pathogens.
For patients with HAP who are being treated empirically and either have a risk factor for MRSA infection (i.e., intravenous antibiotic use within the previous 90 days, hospitalisation where more than 20 percent of S. aureus isolates are methicillin resistant, the prevalence of MRSA is not
known) or who are at a high risk of mortality, the guideline suggests prescribing an antibiotic with activity against MRSA.
Data show that 10 percent of identified HAP cases are caused by methicillin-resistant Staphylococcus aureus (MRSA), whereas about 35 percent are caused by P. aeruginosa and other gram-negative bacilli. "Therefore, coverage for MRSA is indicated only in patients at a high risk of MRSA... or at a high risk of mortality (e.g., those requiring mechanical ventilation or who are in septic shock)," according to the journal article.
In addition, for patients with HAP who are being treated empirically, the guideline recommends prescribing antibiotics with activity against P. aeruginosa and other gram-negative bacilli.
"Patients at a high risk of P. aeruginosa or a high risk of mortality should receive two different classes of antibiotic with activity against P. aeruginosa. Examples include piperacillin-tazobactam, cefepime, levofloxacin, imipenem, and meropenem," the article says.
With regards to duration of treatment for patients with VAP or HAP, the updated guideline recommends a 7-day course, rather than a longer duration, of antimicrobial therapy.
The article authors cite studies on VAP showing that “short courses” of antibiotics (7–8 days) compared with “long courses” (10–15 days) resulted in increased antibiotic-free days but did not affect recurrence of pneumonia, ventilator-free days, duration of mechanical ventilation, length of intensive care unit stay, or mortality.
"There are no recent studies that evaluate the optimal duration of therapy for HAP, so this recommendation is based on the recent data published for VAP," the authors add.
Source: Annals of the American Thoracic Society
Image Credit: Wikimedia Commons
References:
Erb CT, Patel B, Orr J, Bice T,
Richards JB, Metersky ML, Wilson KC, Thomason CC (2016) management of
adults with hospital-acquired and ventilator-associated pneumonia. Ann
Am Thorac Soc, 13(12):2258-2260. DOI: 10.1513/AnnalsATS.201608-641CME
Latest Articles
Hospital-acquired Pneumoniam The American Thoracic Society, Infectious Diseases Society of America, ventilator-associated pneumonia
The American Thoracic Society and the Infectious Diseases Society of America have updated guidelines for the diagnosis and management of hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP)