Patients with septic shock admitted to hospitals affected by the 2011 shortage of the drug norepinephrine had a higher risk of in-hospital death, according to a study presented at the 37th International Symposium on Intensive Care and Emergency Medicine.
See Also: New Strategy for Identifying Sepsis Arising in the ICU
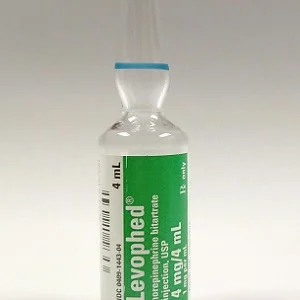
The study, also published in JAMA, examined whether the 2011 drug shortage was associated with changes in care and outcome. Norepinephrine is recommended as the first-line vasopressor (a drug that constricts [narrows] blood vessels, increasing blood pressure) for treatment of hypotension (abnormally low blood pressure) due to septic shock.
The study included 26 U.S. hospitals with a baseline rate of norepinephrine use of at least 60 percent for patients with septic shock. The study group included adults with septic shock admitted to study hospitals between July 2008 and June 2013 (n = 27,835). Hospital-level norepinephrine shortage was defined as any quarterly (3-month) interval in 2011 during which the hospital rate of norepinephrine use decreased by more than 20 percent from baseline.
Among the patients with septic shock in hospitals that demonstrated at least one quarter of norepinephrine shortage in 2011, norepinephrine use declined from 77 percent of patients before the shortage to a low of 56 percent in the second quarter of 2011; phenylephrine was the most frequently used alternative vasopressor during this time. Researchers found that in-hospital mortality increased from 35.9% during non-shortage quarters to 39.6% during shortage quarters, an absolute difference of 3.7% (95% CI,1.5%-6.0%).
"Placing these findings in the context of an estimated 150,000 deaths from sepsis in the United States each year, the norepinephrine shortage observed in 17% of hospitals may have been associated with hundreds of excess deaths," write Hannah Wunsch, MD, MSc, of Sunnybrook Health Sciences Centre, Toronto, and co-authors. "A sustained nationwide shortage of norepinephrine affecting all hospitals in the United States could result in thousands of additional deaths in a year. However, these estimates are based on assumptions that the point estimate represents the true effect size and that the entire difference is causal with no confounding, both of which are speculative."
Several factors may explain the observed associations between norepinephrine shortage and increased patient mortality, including that other specific vasopressors selected to replace norepinephrine may result in worse outcomes for patients with septic shock, and that observable decreases in norepinephrine use in the setting of shortage may be a marker of related unmeasured factors that affected patient outcomes, such as the absence of a dedicated shortage pharmacist to optimise distribution of limited supplies, delayed administration of vasopressors, or lack of clinician familiarity with dosing of alternative vasopressor agents.
Source: JAMA
Image Credit: Mark Oniffrey
Latest Articles
septic shock, Sepsis Deaths, Drug Shortage, norepinephrine
Patients with septic shock admitted to hospitals affected by the 2011 shortage of the drug norepinephrine had a higher risk of in-hospital death, according to a study presented at the 37th International Symposium on Intensive Care and Emergency Medicine.