The harmful side-effects of mechanical ventilation on respiratory muscles are addressed by two recent publications, which provide an overview of the pathophysiology, diagnosis, prevention and possible treatment therapies.
David Berger, Department of Intensive Care Medicine, Inselspital, University Hospital of Bern, Bern, Switzerland and colleagues have reviewed the literature on respiratory muscle weakness and ventilator-induced diaphragmatic dysfunction (VIDD) in the critically ill (Berger et al. 2016). Their article, published in the Journal of Cachexia, Sarcopenia and Muscle, covers the histological and structural changes in the pathophysiology of respiratory muscles dysfunction and how this translates to the patient’s bedside. The main pathophysiological changes are disuse atrophy and microstructural changes, which include decreased protein synthesis, increased proteolysis, and oxidative stress, possibly linked to mitochondrial dysfunction.
Various diagnostic and screening tools are available, including assessment of the electrical diaphragmatic activity and ultrasound. There are roles for ventilatory and pharmacological interventions. Berger et al. recommend that prolonged periods of complete diaphragmatic rest be avoided and diaphragmatic contractions preserved whenever possible. Their literature review concludes that questions remain about the optimal strategy and mode of mechanical ventilation for affected patients. They suggest that effort adapted ventilation modes may offer advantages, but it remains to be seen if this might lead to improved clinical outcomes.
See Also: Diaphragmatic Ultrasonography: an Underutilised Tool
Willem-Jan M. Schellekens, from the Department of Anaesthesiology and the Department Intensive Care Medicine, Radboud University Medical Centre, Nijmegen, the Netherlands, and colleagues address strategies for prevention of respiratory muscle weakness and improving function if weakness has already developed (Schellekens et al. 2016). They focus on interventions that are most likely to be of clinical importance in the near future.
As no specific preventive or therapeutic interventions have been tested in large randomised controlled trials (RCTs) Schellekens et al. recommend those interventions that make sense physiologically or are supported by small clinical studies. Their recommendations are summarised in Figure 2 in the article (reproduced below - CC by 4.0). They note that the rescue interventions are for exceptional cases and should be discussed with the patient or surrogate decision makers.
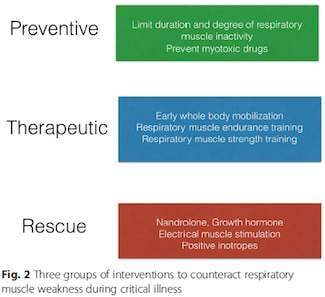
Reproduced from Schelleken et al. (2016)
Schellekens et al. recommend limiting the duration of controlled mechanical ventilation and preventing high levels of support under assisted ventilation in order to reduce the risk of disuse atrophy. They acknowledge that in severe ARDS controlled mechanical ventilation is preferred to facilitate lung-protective ventilation. They outline monitoring techniques to detect complete inactivity of the respiratory muscles due to over-assist.
Inspiratory muscle training is feasible and safe in difficult to wean patients with respiratory muscle weakness who are difficult to wean from the ventilator, they write. They add that it is reasonable to combine inspiratory muscle strength training (IMST) with endurance training in stable, difficult-to-wean patients with confirmed respiratory muscle weakness. However, more research is needed into the best protocol and timing for IMST. Therapies which are not supported by data include antioxidants and other specific feeding strategies, and administration of ß-adrenoreceptor agonists. Anabolic hormones should not be used in the early stage of ICU admission but may have a role in more chronic and stable difficult-to-wean ICU patients with respiratory muscle weakness.
Future therapies Schellekens et al. consider include modulation of inflammation and modulation of proteolytic pathways. For inflammation, human data is scarce and disappointing, they write, while modulation of the proteolytic system is a potentially of interest.
Image credit: Pixabay
David Berger, Department of Intensive Care Medicine, Inselspital, University Hospital of Bern, Bern, Switzerland and colleagues have reviewed the literature on respiratory muscle weakness and ventilator-induced diaphragmatic dysfunction (VIDD) in the critically ill (Berger et al. 2016). Their article, published in the Journal of Cachexia, Sarcopenia and Muscle, covers the histological and structural changes in the pathophysiology of respiratory muscles dysfunction and how this translates to the patient’s bedside. The main pathophysiological changes are disuse atrophy and microstructural changes, which include decreased protein synthesis, increased proteolysis, and oxidative stress, possibly linked to mitochondrial dysfunction.
Various diagnostic and screening tools are available, including assessment of the electrical diaphragmatic activity and ultrasound. There are roles for ventilatory and pharmacological interventions. Berger et al. recommend that prolonged periods of complete diaphragmatic rest be avoided and diaphragmatic contractions preserved whenever possible. Their literature review concludes that questions remain about the optimal strategy and mode of mechanical ventilation for affected patients. They suggest that effort adapted ventilation modes may offer advantages, but it remains to be seen if this might lead to improved clinical outcomes.
See Also: Diaphragmatic Ultrasonography: an Underutilised Tool
Willem-Jan M. Schellekens, from the Department of Anaesthesiology and the Department Intensive Care Medicine, Radboud University Medical Centre, Nijmegen, the Netherlands, and colleagues address strategies for prevention of respiratory muscle weakness and improving function if weakness has already developed (Schellekens et al. 2016). They focus on interventions that are most likely to be of clinical importance in the near future.
As no specific preventive or therapeutic interventions have been tested in large randomised controlled trials (RCTs) Schellekens et al. recommend those interventions that make sense physiologically or are supported by small clinical studies. Their recommendations are summarised in Figure 2 in the article (reproduced below - CC by 4.0). They note that the rescue interventions are for exceptional cases and should be discussed with the patient or surrogate decision makers.
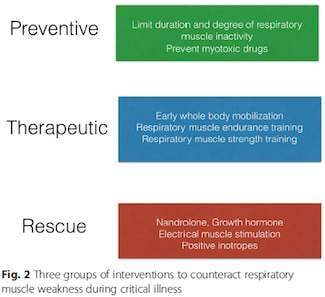
Reproduced from Schelleken et al. (2016)
Schellekens et al. recommend limiting the duration of controlled mechanical ventilation and preventing high levels of support under assisted ventilation in order to reduce the risk of disuse atrophy. They acknowledge that in severe ARDS controlled mechanical ventilation is preferred to facilitate lung-protective ventilation. They outline monitoring techniques to detect complete inactivity of the respiratory muscles due to over-assist.
Inspiratory muscle training is feasible and safe in difficult to wean patients with respiratory muscle weakness who are difficult to wean from the ventilator, they write. They add that it is reasonable to combine inspiratory muscle strength training (IMST) with endurance training in stable, difficult-to-wean patients with confirmed respiratory muscle weakness. However, more research is needed into the best protocol and timing for IMST. Therapies which are not supported by data include antioxidants and other specific feeding strategies, and administration of ß-adrenoreceptor agonists. Anabolic hormones should not be used in the early stage of ICU admission but may have a role in more chronic and stable difficult-to-wean ICU patients with respiratory muscle weakness.
Future therapies Schellekens et al. consider include modulation of inflammation and modulation of proteolytic pathways. For inflammation, human data is scarce and disappointing, they write, while modulation of the proteolytic system is a potentially of interest.
Image credit: Pixabay
References:
Berger D, Bloechlinger S, von Haehling S, Doehner W, Takala J,
Z'Graggen WJ, Schefold JC (2016) Dysfunction of respiratory muscles in critically ill patients on the intensive care unit. J Cachexia
Sarcopenia Muscle, Mar 9. doi: 10.1002/jcsm.12108. [Epub ahead of print]
Schellekens WJ, van Hees HW, Doorduin J, Roesthuis LH, Scheffer GJ, van der Hoeven JG, Heunks LM (2016) Strategies to optimize respiratory muscle function in ICU patients. Crit Care, 20(1):103. doi: 10.1186/s13054-016-1280-y.
Schellekens WJ, van Hees HW, Doorduin J, Roesthuis LH, Scheffer GJ, van der Hoeven JG, Heunks LM (2016) Strategies to optimize respiratory muscle function in ICU patients. Crit Care, 20(1):103. doi: 10.1186/s13054-016-1280-y.
Latest Articles
respiratory muscles, weakness, ICU
The harmful side-effects of mechanical ventilation on respiratory muscles are addressed by two recent publications, which provide an overview of the pathophysiology, diagnosis, prevention and possible treatment therapies.