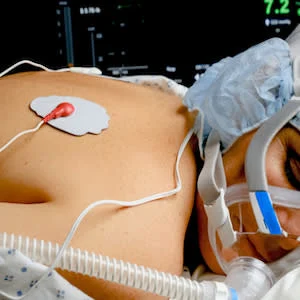
The COVID-19 pandemic has placed unprecedented stress on health care institutions everywhere. Among other interventions, researchers and physicians have been trying to reevaluate the use of mechanical ventilation. The rise of social media has accelerated the spread of biased information about therapies that have not been peer-reviewed and have little to no evidence about its efficacy. Therefore, the question is whether or not traditional scientific rigour should continue to be employed in the face of the pandemic to look for low-tech, low-cost therapeutic interventions? One such intervention is the use of prone positioning in non-intubated patients.
Prone positioning has been established to have positive outcomes on mortality when patients have mild to severe acute respiratory distress (ARDS) and are placed on ventilators. However, patients with mild ARDS do not enjoy any decrease in mortality despite better oxygenation achieved on prone positioning.
A study conducted from March 20 to April 9, 2020, found that prone positioning of study participants for at least 3 hours significantly improved oxygen saturation. After they were placed back in the supine position, half (n=23) of the participants could not maintain their oxygen saturation levels. Similarly, there was no difference observed in intubation rates between responders (patients who maintained oxygen saturation) and non-responders (patients who did not maintain oxygen saturation) on resupination. What should we conclude from the study results?
In theory, it appears that a simple, zero-cost manoeuvre such as prone positioning can improve oxygen saturation and prevent ventilator-associated lung injuries. In reality, research evidence from other ARDS trials has shown that improved oxygen saturation levels do not affect the rates of people requiring mechanical ventilation or a decrease in mortality.
Despite research evidence that lung-protective ventilation benefits the patients, it has not been used in intensive care units in a uniform fashion. It is well known that the adoption of research evidence from rigorous scientific studies is not readily adopted in community practice.
At the same time, given the desperation associated with COVID-19 and widespread dissemination of misleading information on therapeutic interventions on social media, clinicians have been found to be using therapeutic choices with no evidence base. It has also been seen that even after the information is found to be misleading, clinicians continue to use them. The quick uptake of positioning in non-intubated COVID-19 patients in a prone position is a good example of how anecdotal evidence spread by social media can influence clinical decision making.
It is important to note that there is a recognition of a difference between adopting an intervention as an emergency measure in resource-poor settings and the adoption of nonevidence-based protocols in daily practice.
Health care providers need to stick to interventions that have been proven effective through rigorous scientific studies. Even these uncertain and stressful times do not warrant lowering our standards by adopting anecdotal evidence, even if they appear relatively harmless. There is a long history of interventions that appear to make sense but have been disproved in randomised controlled trials.
Source: The Lancet
Image Credit: iStock
References:
Munshi et al. (2020) Prone positioning in non-intubated patients with COVID-19: raising the bar. The Lancet. doi.org/10.1016/S2213-2600(20)30269-1
Latest Articles
Prone positioning, COVID-19, non-intubated
Prone Positioning in Non-Intubated COVID-19 Patients