A recent study has found an association between baseline P-wave morphology and subsequent ischemic stroke risk. The study was led by Hooman Kamel, MD, Department of Neurology, Weill Cornell Medical College, New York. It was published online in Stroke.
Emerging data already suggests that left atrial disease may be a cause of ischemic stroke in the absence of AF and may be a cause for many strokes classified as cryptogenic. The objective of the study was to examine the association between P-wave morphology and stroke while accounting for incident atrial fibrillation (AF).
The study titled the Multi-Ethnic Study of Atherosclerosis (MESA) enrolled 6814 men and women between the ages of 45 to 84 years. The participants were free from any apparent cerebrovascular or cardiovascular disease, including AF. Incident AF was accounted for during the study as were age, sex, race, hypertension, left ventricular hypertrophy, cholesterol level, lipoprotein levels, diabetes, chronic obstructive pulmonary disease, chronic kidney disease, body mass index and smoking status.
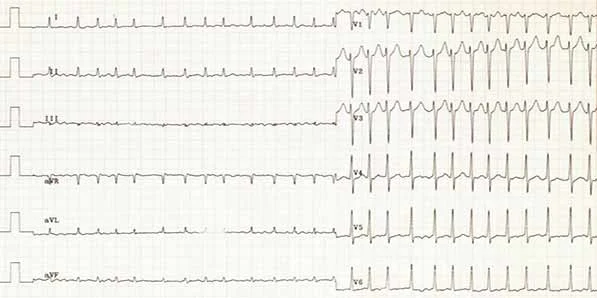
Study researchers obtained 12-lead ECG from each patient's first and last study visit. Each patient's P-wave areas, amplitudes and durations were measured. The authors of the study defined P-wave terminal force in lead V1 (PTFV1) as the duration (in ms) of the downward deflection of the P wave in lead V1 multiplied by the absolute value of its amplitude.
Study participants were followed for a median of 8.5 years. During this time frame, ischemic stroke occurred in 121 patients. PTFV1 was found to be more strongly associated with incident stroke than with incident AF. Association between PTFV1 and stroke was similar for incident AF.
During the study period, it was observed that the association between PTFV1 and subsequent ischemic stroke persisted in participants even without any AF. The findings thus suggest that atrial disease may cause stroke even without the presence of AF. The findings also help explain cryptogenic strokes.
The authors of the study conclude that "P-wave area and terminal force are associated with stroke risk, but did not control for AF, which may mediate the relationship between P-wave morphology and stroke."
Further research is still required to fully understand this association. The authors of the study indicate that they may have missed subclinical AF that could have mediated the association between PTFV1 and stroke. The researchers were also unable to examine the association with embolic-appearing or cryptogenic stroke as well as assess the interaction between ethnicity and P-wave morphology with the risk of stroke. No imaging of the left atrium was performed during this study but the researchers do point out that P-wave measurements are not necessarily captured by imaging data.
However, work still needs to be done to fully delineate the ECG, imaging and biomarker characteristics of atrial cardiopathy. AF may be an imperfect marker of risk and a study of a combination of markers may help understand the risk of left atrial embolization better.
Source: Medscape
Image credit: Wikimedia Commons
Emerging data already suggests that left atrial disease may be a cause of ischemic stroke in the absence of AF and may be a cause for many strokes classified as cryptogenic. The objective of the study was to examine the association between P-wave morphology and stroke while accounting for incident atrial fibrillation (AF).
The study titled the Multi-Ethnic Study of Atherosclerosis (MESA) enrolled 6814 men and women between the ages of 45 to 84 years. The participants were free from any apparent cerebrovascular or cardiovascular disease, including AF. Incident AF was accounted for during the study as were age, sex, race, hypertension, left ventricular hypertrophy, cholesterol level, lipoprotein levels, diabetes, chronic obstructive pulmonary disease, chronic kidney disease, body mass index and smoking status.
Study researchers obtained 12-lead ECG from each patient's first and last study visit. Each patient's P-wave areas, amplitudes and durations were measured. The authors of the study defined P-wave terminal force in lead V1 (PTFV1) as the duration (in ms) of the downward deflection of the P wave in lead V1 multiplied by the absolute value of its amplitude.
Study participants were followed for a median of 8.5 years. During this time frame, ischemic stroke occurred in 121 patients. PTFV1 was found to be more strongly associated with incident stroke than with incident AF. Association between PTFV1 and stroke was similar for incident AF.
During the study period, it was observed that the association between PTFV1 and subsequent ischemic stroke persisted in participants even without any AF. The findings thus suggest that atrial disease may cause stroke even without the presence of AF. The findings also help explain cryptogenic strokes.
The authors of the study conclude that "P-wave area and terminal force are associated with stroke risk, but did not control for AF, which may mediate the relationship between P-wave morphology and stroke."
Further research is still required to fully understand this association. The authors of the study indicate that they may have missed subclinical AF that could have mediated the association between PTFV1 and stroke. The researchers were also unable to examine the association with embolic-appearing or cryptogenic stroke as well as assess the interaction between ethnicity and P-wave morphology with the risk of stroke. No imaging of the left atrium was performed during this study but the researchers do point out that P-wave measurements are not necessarily captured by imaging data.
However, work still needs to be done to fully delineate the ECG, imaging and biomarker characteristics of atrial cardiopathy. AF may be an imperfect marker of risk and a study of a combination of markers may help understand the risk of left atrial embolization better.
Source: Medscape
Image credit: Wikimedia Commons
Latest Articles
ischemic stroke, ECG, AF, P-wave morphology, PTFV1
A recent study has found an association between baseline P-wave morphology and subsequent ischemic stroke risk. The study was led by Hooman Kamel, MD, Depa...