New research from Norway shows that out-of-hospital cardiac arrest (OHCA) survival was higher in urban compared to rural areas. To save more lives following OHCA, continuous endeavours to optimise modifiable prehospital factors (e.g., bystander CPR and response time) are required to improve every link in the chain of survival, according to the study published in the journal Critical Care.
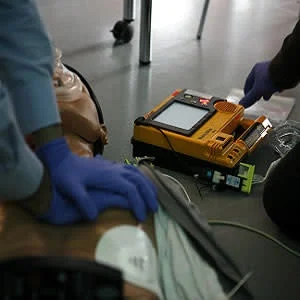
OHCA is a major cause of death in industrialised countries, and survival differs substantially worldwide. Survival is associated with certain OHCA patient factors, but these are generally non-modifiable. However, some prehospital system factors in OHCA such as bystander cardiopulmonary resuscitation (CPR), emergency medical services (EMS) response times, and the attendance of EMS physicians, are modifiable. These factors represent opportunities for improvements in saving lives, the study authors say.
The study aimed to examine how bystander CPR, EMS response time, and EMS physician attendance influence survival at different stages of care, and to what extent this differs between rural and urban areas. The study included 1,138 medical OHCA patients from an Utstein template-based cardiac arrest registry. Kaplan-Meier type survival curves, univariable and multivariable logistic regression and mortality hazard plots were used for analysis of study data. Key findings include:
- There was a significantly higher probability for survival to hospital admission (OR: 1.84, 95% CI 1.43–2.36, p < 0.001), to hospital discharge (OR: 1.51, 95% CI 1.08–2.11, p = 0.017), and at 1 year (OR: 1.58, 95% CI 1.11–2.26, p = 0.012) in the urban group versus the rural group.
- In patients receiving bystander CPR before EMS arrival, the odds of survival to hospital discharge increased more than threefold (OR: 3.05, 95% CI 2.00–4.65, p < 0.001). However, bystander CPR was associated with increased patient survival to discharge only in urban areas (survival probability 0.26 with CPR vs. 0.08 without CPR, p < 0.001).
- EMS response time ≥ 10 min was associated with decreased survival (OR: 0.61, 95% CI 0.45–0.83, p = 0.002), however, only in urban areas (survival probability 0.15 ≥ 10 min vs. 0.25 < 10 min, p < 0.001).
- In rural areas, patients with EMS physician attendance had an overall better survival to hospital discharge (survival probability 0.17 with EMS physician vs. 0.05 without EMS physician, p = 0.019).
After adjusting for modifiable factors, the survival differences remained, the authors noted.
"The higher OHCA survival in urban compared to rural areas found in the present study corresponds with the results of previous reports. Still, among patients admitted alive, our results indicate no significant difference in later mortality, whether in the emergency department, 24 hours after hospital admission, mortality at hospital discharge, or at 1 year," the authors wrote." This is an important finding, and to our knowledge not reported before. It implies that further overall improvement in survival in rural areas must be based on community-based interventions."
Specifically, rural communities need to strengthen CPR training, implement first-responder programmes and have public access defibrillators. With implementation of best practice, survival following OHCA could also be improved, the authors added.
Source: Critical Care
Image Credit: Rama
References:
Mathiesen WT et al. (2018) Effects of modifiable prehospital factors on survival after out-of-hospital cardiac arrest in rural versus urban areas. Critical Care 18 April 2018. 22:99 https://doi.org/10.1186/s13054-018-2017-x
Latest Articles
out-of-hospital cardiac arrest, OHCA, community-based interventions, CPR training
New research from Norway shows that out-of-hospital cardiac arrest (OHCA) survival was higher in urban compared to rural areas. To save more lives following OHCA, continuous endeavours to optimise modifiable prehospital factors (e.g., bystander CPR and re