Intensivists need to learn from their oncologist colleagues by running trials with carefully selected patient groups, as medicine moves from personalised medicine to precision medicine, said Prof Jean-Louis Vincent, speaking at the opening of the 38th International Symposium on Intensive Care and Emergency Medicine in Brussels on Tuesday.
We need more studies, he said, but we need more good studies. Randomised controlled trials should not be an aim, they are the means to address a valid question. It sometimes seems like people decide on a RCT then find a topic, he observed. Any abnormality is associated with worse outcomes, statistically speaking, when it comes to trials, he added.
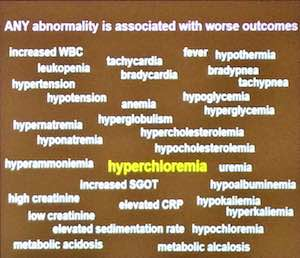
Vincent outlined his concerns with trials comparing saline with other fluids. There’s a simple syllogism: a liberal infusion of saline solutions results in hyperchloremia and hyperchloremia cannot be good (especially for the kidneys. So we should not use saline solutions liberally, and too little fluid cannot show any toxicity. Should we hurt some patients to demonstrate this, he asked. The SPLIT trial already indicated the problem with saline solutions - hyperchloremia - and the blood chloride levels in the patients were not measured. Comparing two intravenous solutions with different compositions makes no sense as he and DeBacker have argued.
The message is that we must monitor serum chloride levels. If you give saline (in the absence of metabolic acidosis) limit it to one litre. If you want to give more than one litre check electrolytes after each litre. Stop giving saline in case of hyperchloremia (chloride levels above 105 mEq/L).
Many multicentric RCTs targeting mortality have shown no difference, e.g. glucose control, activated protein C, blood transfusions, time of onset of RRT, albumin administration and so on. And others have shown harm, e.g. early parenteral nutrition, mechanical ventilation, HES solutions, large tidal volumes and so on. We may even need to consider whether we need RCTs at all, e.g. for extracorporeal membrane oxygenation (ECMO).
Some trials report benefits for subgroups, in which case why don’t you individualise the treatment, suggested Vincent. With such a heterogeneous patient population, intensivists need to individualise metabolic support or drug therapy rather than wait to enrol patients in RCTs. Even with trials split by patient types e.g. medical or surgical ICU patients, or ARDS patients, the time course of events can follow a very complex evolution regardless of the primary problem.
The problem with trials is to identify the right type of patients even if that means the number of patients goes down. Secondly we need to reconsider outcomes, to include not only mortality but organ function over time, which has been shown to be more meaningful.
Intensive care needs to move away from trials with poorly characterised patient populations, emphasised Vincent and advance towards personalised medicine and eventually to precision medicine as in the 3P model.