Existing critical care is expensive, poorly distributed and severely stretched. Regionalised trauma centres have shown mortality benefits, so should critical care be regionalised at larger centres? Derek Angus, Alain Combes and Jerry Nolan addressed this vexed question in relation to critical care, ECMO and resuscitation, speaking at the International Symposium on Intensive Care and Emergency Medicine meeting in Brussels last month.
Derek Angus (Pittsburgh, USA) explained that the ideal is to enact a patient-to-care management system, to triage and steer the sickest patients to “supercentres”, on a regional basis. Nguyen et al., in a study published in the American Journal of Respiratory Care and Critical Medicine evaluated three alternative organisational models - regionalisation, telemedicine and community outreach in reorganising adult critical care delivery.
Angus acknowledged that of course this does not mean abandoning care provided everywhere else. The supercentres need to help smaller, lower level centres by means of telemedicine, outreach and training.
What is the rationale for creation of centralised large centres? Angus explained that data from the United States shows high variation in ICU beds per capita. Moran and Scanlon found slow progress in complying to safety standards in intensivist staffing levels. In 2002 58.94 reported to Leapfrog on the intensivist staffing standard, with 14.74 percent fully adopting the standard. In 2007 this rose to 59.45 percent and 21.41 percent respectively - a 6.67 difference in 5 years. Wallace, Angus and colleagues addressed changing ICU supply in a recent article in the American Journal of Respiratory and Critical Care Medicine, which found that national trends in ICU bed growth are not uniformly reflected at the regional level, with most growth occurring in a small number of highly populated regions.
Pronovost et al. published a systematic review in JAMA in 2002 that studied physician staffing patterns and clinical outcomes in critically ill patients, which found that high-intensivy vs low-intensity ICU physician staffing is associated with reduced hospital and ICU mortality and hospital and ICU length of stay. Other studies include that by Wallace et al. in the New England Journal of Medicine in 2012, which found that the addition of nighttime intensivist staffing to a low-intensity daytime staffing model was associated with reduced mortality. However, a reduction in mortality was not seen in ICUs with high-intensity daytime staffing.
MacKenzie et al. in a study published in NEJM 2006 found a benefit to regional trauma centres, with the largest benefits in sickest patients. Mortality for patients treated in trauma centres was 7.6 percent versus 9.5 percent in non-trauma centre hospitals.
Kahn et al. looked at the potential value of regionalised intensive care for mechanically ventilated medical patients in a study published in the American Journal of Respiratory and Critical Care Medicine in 2008. The study looked at the distribution of patients across ICUs and how far you would need to drive. Most patients’ drive time would be less than 20 miles (the median was 8.5 miles), for a 20 percent increase in survival.
Recent evidence is that informal centralisation already exists, according to Wallace et al. in a paper published in PLoS in 2014 on geographic access to high capability severe acute respiratory failure centres in the United States. Furthermore a paper by Seymour ( under review) conducted a simulation study on re-routing ambulances. This made ambulance runs more efficient, if prehospital triage for patients with a critical illness score greater than or equal to 2 were sent to tertiary centres.
Cautioned Angus, regionalisation does have potential benefits. It does not mean abandoning and de-skilling outlying hospitals. On the other hand, systems will need to avoid overloading tertiary centres. There are many other additional considerations before implementing such a regionalised system. Should transport be scene to hospital or inter-hospital? What happens to patients developing critical illness in an outlying hospital? Reiumbursement needs to be worked out, and potential physician resistance addressed. Not least, there are patient and family choices to consider. In the United States there are also competing hospital networks.
Angus concluded by recommending demonstration projects, including regional centres, telemedicine, community outreach and hybrids. There also needs to be ‘mechanism of action’ research into alternative staffing models, and why there is a benefit from volume in relation to outcome.
Alain Combes (Paris, France) argued the case for ECMO centres, outlining why only experienced teams will be able to prevent or detection early enough severe ECMO-associated complications. Veno-Arterial (VA) ECMO should be conducted in association with a heart surgery centre with a heart transplant programme. Veno-venous (VV) ECMO shares many of the complications of VA ECMO. Patients on VV may be switched to VA and vice versa. Such specialisation exists in Paris, France as well as in Italy, Australia and other countries. Only experienced centres should run ECMO programmes. Such centres need to see both VA and VV, at least 20 cases per year, and be staffed by experienced physicians, nurses and perfusionists. Combes advised that there should regional networks of hospitals, which can detect early refractory cardiac/ respiratory failure. All ECMO centres should have mobile ECMO retrieval teams available 24/7. He asked the audience, "Would you go for coronary artery bypass grafting surgery to a centre which performs fewer than 100 cases per year?"
Oliver Grottke (Aachen, Germany) described the trauma system in Germany - the system mantra is to get the patient to the right place, at the right time for the right treatment. Centralising trauma care may optimise patient treatment. For trauma patients, evidence showing the benefit of centralised care stacked up early due to the experience of the military, and civilian evidence for trauma centres was published in the U.S. as early as 1979 (West & Trunkey). This study was the first indication that centralised, aggressive intervention by experienced personnel could potentially reduce mortality rate resulting from injury. In the UK specialised trauma centres were proposed, after a retrospective review in 1988 found that more than thirty percent were potentially preventable. In addiiton, significant inter-hospital variation in mortality rates was observed. The first European study to find a positive effect of inclusive trama care systems on in-hospital mortality was published by Twinjstra et al. in the Annals of Surgery, which found a statistically significant risk reduction of death of 16 percent. Similar benefits were found in Australia, with the authors of the Australian study concluding that “Such inclusive systems of trauma care should be regarded as a minimum standard for health jurisdictions.”
The evidence of the benefits of centralised trauma centres is that specialist units aim to provide better care for patients, have more efficient use of existing resources, have the skills, experience and specialist equipment readily accessible, patients experience less need for transit to another hospital (and reduced transit time may be crucial to survival), and more lives are likely to be saved and quality of life improved as the risk of permanent disability and lengthy hospital stays are reduced.
Centralised trauma care requires initial assessment and triage to determine necessary treatment and where the patient should be treated e.g. burns unit, cardiac centre etc. Like Angus, Grottke recommends regionalised care, as a single major trauma centre is not always suitable, for example for dispersed, rural populations. Centralisation may result in over triage and selective triage, patient “dumping” and loss of skills in smaller facilities.
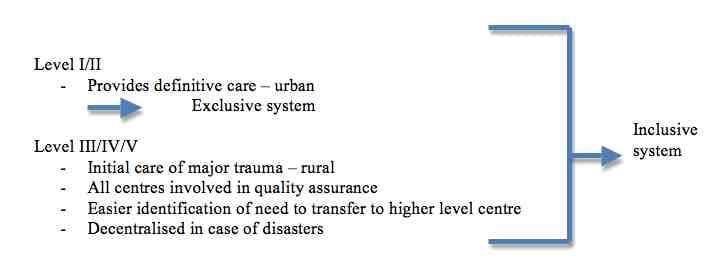
Inclusive trauma systems improve patient outcomes, and severely injured patients have greater inpatient survival. Triage to a trauma centre is similar in both inclusive and exclusive systems, showing that patients are receiving appropriate treatment in both systems. Grottke noted that current recommendations from the American College of Surgeons advocates the integration of suitable levels of trauma centre as part of an inclusive system.
What are the critical components of a trauma system? From the literature (Lendrum and Lockey 2013) and Kanakaris and Giannoudis 2011, Grottke noted that these are:
In considering centralisation, Grottke cautioned there were issues to consider. Centralisation may be hampered by constraints of staff, space and cost. If local hospitals lose specialist services they may be less sustainable and there may be an impact on patient morbidity. One size may not fit all, as different areas may require different facilities, for example between urban and rural areas.
Jerry Nolan (Bath, UK) made the case for cardiac arrest centres to maximise myocardical and neurological recovery, comparing outcomes from trauma centres to the potential for centralising cardiac arrest centres. Nolan suggested that such centres were a logical progression of existing regionalisation. They need 24/7 access to a cardiac cath lab, comprehensive post-resuscitation care and neurological support for prognostication. Indirect evidence is that they lead to better outcomes.
Derek Angus (Pittsburgh, USA) explained that the ideal is to enact a patient-to-care management system, to triage and steer the sickest patients to “supercentres”, on a regional basis. Nguyen et al., in a study published in the American Journal of Respiratory Care and Critical Medicine evaluated three alternative organisational models - regionalisation, telemedicine and community outreach in reorganising adult critical care delivery.
Angus acknowledged that of course this does not mean abandoning care provided everywhere else. The supercentres need to help smaller, lower level centres by means of telemedicine, outreach and training.
What is the rationale for creation of centralised large centres? Angus explained that data from the United States shows high variation in ICU beds per capita. Moran and Scanlon found slow progress in complying to safety standards in intensivist staffing levels. In 2002 58.94 reported to Leapfrog on the intensivist staffing standard, with 14.74 percent fully adopting the standard. In 2007 this rose to 59.45 percent and 21.41 percent respectively - a 6.67 difference in 5 years. Wallace, Angus and colleagues addressed changing ICU supply in a recent article in the American Journal of Respiratory and Critical Care Medicine, which found that national trends in ICU bed growth are not uniformly reflected at the regional level, with most growth occurring in a small number of highly populated regions.
Pronovost et al. published a systematic review in JAMA in 2002 that studied physician staffing patterns and clinical outcomes in critically ill patients, which found that high-intensivy vs low-intensity ICU physician staffing is associated with reduced hospital and ICU mortality and hospital and ICU length of stay. Other studies include that by Wallace et al. in the New England Journal of Medicine in 2012, which found that the addition of nighttime intensivist staffing to a low-intensity daytime staffing model was associated with reduced mortality. However, a reduction in mortality was not seen in ICUs with high-intensity daytime staffing.
MacKenzie et al. in a study published in NEJM 2006 found a benefit to regional trauma centres, with the largest benefits in sickest patients. Mortality for patients treated in trauma centres was 7.6 percent versus 9.5 percent in non-trauma centre hospitals.
Kahn et al. looked at the potential value of regionalised intensive care for mechanically ventilated medical patients in a study published in the American Journal of Respiratory and Critical Care Medicine in 2008. The study looked at the distribution of patients across ICUs and how far you would need to drive. Most patients’ drive time would be less than 20 miles (the median was 8.5 miles), for a 20 percent increase in survival.
Recent evidence is that informal centralisation already exists, according to Wallace et al. in a paper published in PLoS in 2014 on geographic access to high capability severe acute respiratory failure centres in the United States. Furthermore a paper by Seymour ( under review) conducted a simulation study on re-routing ambulances. This made ambulance runs more efficient, if prehospital triage for patients with a critical illness score greater than or equal to 2 were sent to tertiary centres.
Cautioned Angus, regionalisation does have potential benefits. It does not mean abandoning and de-skilling outlying hospitals. On the other hand, systems will need to avoid overloading tertiary centres. There are many other additional considerations before implementing such a regionalised system. Should transport be scene to hospital or inter-hospital? What happens to patients developing critical illness in an outlying hospital? Reiumbursement needs to be worked out, and potential physician resistance addressed. Not least, there are patient and family choices to consider. In the United States there are also competing hospital networks.
Angus concluded by recommending demonstration projects, including regional centres, telemedicine, community outreach and hybrids. There also needs to be ‘mechanism of action’ research into alternative staffing models, and why there is a benefit from volume in relation to outcome.
Alain Combes (Paris, France) argued the case for ECMO centres, outlining why only experienced teams will be able to prevent or detection early enough severe ECMO-associated complications. Veno-Arterial (VA) ECMO should be conducted in association with a heart surgery centre with a heart transplant programme. Veno-venous (VV) ECMO shares many of the complications of VA ECMO. Patients on VV may be switched to VA and vice versa. Such specialisation exists in Paris, France as well as in Italy, Australia and other countries. Only experienced centres should run ECMO programmes. Such centres need to see both VA and VV, at least 20 cases per year, and be staffed by experienced physicians, nurses and perfusionists. Combes advised that there should regional networks of hospitals, which can detect early refractory cardiac/ respiratory failure. All ECMO centres should have mobile ECMO retrieval teams available 24/7. He asked the audience, "Would you go for coronary artery bypass grafting surgery to a centre which performs fewer than 100 cases per year?"
Oliver Grottke (Aachen, Germany) described the trauma system in Germany - the system mantra is to get the patient to the right place, at the right time for the right treatment. Centralising trauma care may optimise patient treatment. For trauma patients, evidence showing the benefit of centralised care stacked up early due to the experience of the military, and civilian evidence for trauma centres was published in the U.S. as early as 1979 (West & Trunkey). This study was the first indication that centralised, aggressive intervention by experienced personnel could potentially reduce mortality rate resulting from injury. In the UK specialised trauma centres were proposed, after a retrospective review in 1988 found that more than thirty percent were potentially preventable. In addiiton, significant inter-hospital variation in mortality rates was observed. The first European study to find a positive effect of inclusive trama care systems on in-hospital mortality was published by Twinjstra et al. in the Annals of Surgery, which found a statistically significant risk reduction of death of 16 percent. Similar benefits were found in Australia, with the authors of the Australian study concluding that “Such inclusive systems of trauma care should be regarded as a minimum standard for health jurisdictions.”
The evidence of the benefits of centralised trauma centres is that specialist units aim to provide better care for patients, have more efficient use of existing resources, have the skills, experience and specialist equipment readily accessible, patients experience less need for transit to another hospital (and reduced transit time may be crucial to survival), and more lives are likely to be saved and quality of life improved as the risk of permanent disability and lengthy hospital stays are reduced.
Centralised trauma care requires initial assessment and triage to determine necessary treatment and where the patient should be treated e.g. burns unit, cardiac centre etc. Like Angus, Grottke recommends regionalised care, as a single major trauma centre is not always suitable, for example for dispersed, rural populations. Centralisation may result in over triage and selective triage, patient “dumping” and loss of skills in smaller facilities.
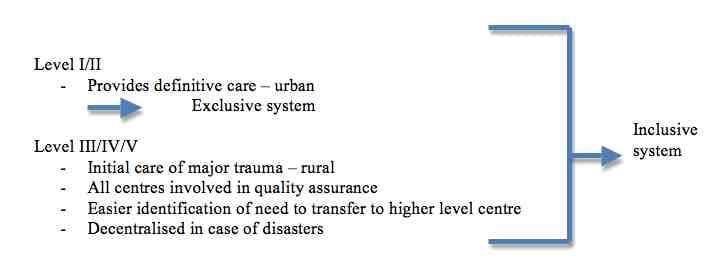
Inclusive trauma systems improve patient outcomes, and severely injured patients have greater inpatient survival. Triage to a trauma centre is similar in both inclusive and exclusive systems, showing that patients are receiving appropriate treatment in both systems. Grottke noted that current recommendations from the American College of Surgeons advocates the integration of suitable levels of trauma centre as part of an inclusive system.
What are the critical components of a trauma system? From the literature (Lendrum and Lockey 2013) and Kanakaris and Giannoudis 2011, Grottke noted that these are:
- Leadership
- Trauma care facilities
- Human resources including 24-hour consultant presence
- Education/ public awareness, including information on the trauma system and communication pathways with primary care and the public). Education for staff should include trauma-related as well as non-technical skills
- Triage-Transport means, including communication network. Suitable coverage of the region is required, including minimum transfer times to trauma centres.
- Rehabilitation, data collection and quality assurance monitoring
- Minimum annual intake is needed at each centre so that the necessary levels of readiness and expertise are maintained.
In considering centralisation, Grottke cautioned there were issues to consider. Centralisation may be hampered by constraints of staff, space and cost. If local hospitals lose specialist services they may be less sustainable and there may be an impact on patient morbidity. One size may not fit all, as different areas may require different facilities, for example between urban and rural areas.
Jerry Nolan (Bath, UK) made the case for cardiac arrest centres to maximise myocardical and neurological recovery, comparing outcomes from trauma centres to the potential for centralising cardiac arrest centres. Nolan suggested that such centres were a logical progression of existing regionalisation. They need 24/7 access to a cardiac cath lab, comprehensive post-resuscitation care and neurological support for prognostication. Indirect evidence is that they lead to better outcomes.
Latest Articles
trauma, cardiac arrest, intensive care, ISICEM 2015, #ISICEM15, Centralisation, Regionalisation
Existing critical care is expensive, poorly distributed and severely stretched. Regionalised trauma centres have shown mortality benefits, so should critic...