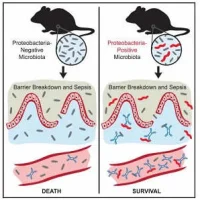
Patients admitted to intensive care units are mostly suffering from sepsis, septic shock, traumatic haemorrhagic shock (HTS), and traumatic brain injury (TBI). It is known that gaseous messengers, especially nitric oxide (NO) and carbon monoxide (CO), play a key role in those life threatening pathological situations. A review paper, published by Frontiers in Medicine, discusses the mechanisms that are associated with the modulation of mitochondrial function mediated by NO and CO, which may critically influence the outcome of patients with critical care diseases.
"In critical care diseases (CCD), two major pathological processes are operating, namely, impaired tissue perfusion causing tissue hypoxia and induction of an inflammatory host response either in a septic or in an aseptic way. Both processes have been shown to induce NO and CO generation," according to the paper authored by Dr. J. Catharina Duvigneau (Department of Biomedical Sciences, University of Veterinary Medicine, Vienna, Austria) and Dr. Andrey V. Kozlov (Ludwig Boltzmann Institute for Experimental and Clinical Traumatology, Vienna).
The outcome of patients with CCD such as sepsis, haemorrhagic shock, or trauma is often associated with mitochondrial dysfunction. In turn, mitochondrial dysfunction is frequently induced upon interaction with NO and CO, two gaseous messengers formed in the body by NO synthase (NOS) and heme oxygenase (HO), respectively. A multitude of factors that are associated with the pathology of CCD exert a potential to interfere with mitochondrial function or the effects of the gaseous messengers, the paper says.
"Although analyses of mitochondrial function in patients with CCD are limited due to the restricted availability of samples, the results of these studies point towards a critical contribution of mitochondrial dysfunction to deleterious outcome," the authors explain.
As shown in previous studies of patients suffering from septic shock, mitochondrial dysfunction was most pronounced in non-survivors. It was also suggested that not only mitochondrial dysfunction but also a decreased mitochondrial content may compromise bioenergetics status of respective tissues. However, mitochondrial function/dysfunction appears to vary substantially among subjects suffering from CCD, organs are affected to a different degree, and mitochondrial function/dysfunction may change during disease progression, according to the authors.
Drs. Duvigneau and Kozlov say the result of interaction between gaseous mediators and mitochondria is predominantly defined by the following four conditions:
• The enzymatic systems generating gaseous messengers are often dysregulated under hypoxia and inflammation. If produced in excess, they compete for the O2-binding sites and may substantially impair mitochondrial respiration.
• O2 saturation of tissues and mitochondrial access to O2 is frequently limited in CCD. Thus, the effects of CO and NO are more pronounced at low O2 concentrations. Vice versa, increased O2 levels will weaken the effects of the gaseous messengers. Apart from mitochondrial proteins, gaseous messengers can also directly influence gene expression via reaction with heme-containing transcription factors and thereby activate mitochondrial biogenesis.
• Redox state of the cell and mitochondria is frequently severely deranged. Changes in the redox environment of the cell are able to influence the interaction of gaseous messengers with mitochondria. CO is not redox active, and its effects are not likely influenced by redox status. By contrast, NO is redox active and can generate further products, which have quite different chemical properties than NO itself. NO reacts with superoxide to form ONOO, which is a strong pro-oxidative molecule inducing oxidative stress, and irreversibly damages complex I, aconitase, and a number of other mitochondrial proteins. It can also damage mitochondrial membrane and uncouple mitochondria.
• Frequently a dysregulation of the acid/base balance toward acidosis is determined in CCD. Hypoxia/ischaemia leads to an enhanced anaerobic glycolysis due to the scarcity of oxygen. The resulting increased production of lactate is associated with a decrease in tissue pH. Lower pH favours the formation of nitric acid from nitrite, the end product of the NO catabolism. Under acidic conditions, nitric acid can disproportionate and thereby release NO. Therefore, NO concentration is higher in acidic hypoxic tissues.
In conclusion, the authors say the mitochondria mediated actions of NO and CO can be both deleterious and beneficial. The effects of NO/CO are dependent on the balance between the NO/CO generation and elimination rates, ongoing inflammatory responses, and the generated reactive oxygen species (ROS) as well as the depth of tissue hypoxia.
Source: Frontiers in Medicine
Image Credit: US Army
References:
Duvigneau, J. Catharina et al. (2017) Pathological Impact of the Interaction of NO and CO with Mitochondria in Critical Care Diseases. Frontiers in Medicine. doi.org/10.3389/fmed.2017.00223
Latest Articles
Sepsis, intensive care units, mitochondrial function, traumatic haemorrhagic shock
Patients admitted to intensive care units are mostly suffering from sepsis, septic shock, traumatic haemorrhagic shock (HTS), and traumatic brain injury (TBI). It is known that gaseous messengers, especially nitric oxide (NO) and carbon monoxide (CO), pla