Brain injury is a leading cause of death among patients who are hospitalised after cardiac arrest (CA). A large majority of these patients die following withdrawal of life sustaining therapy (WLST) due to poor neurological prognosis. A multimodal prognostication approach may be needed so that the results of a clinical neurological examination can be considered together with the findings of electrophysiological investigations, serum biomarkers and neuroimaging.
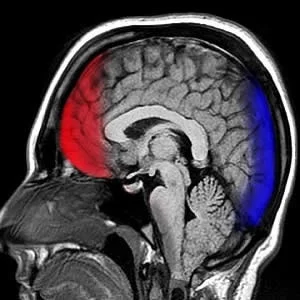
Findings from a large European survey show that head computed tomography (CT) and EEG are the two most frequently used methods for prognostication. CT offers several benefits. It is widely available and is also cheaper and easier to perform on ICU patients when compared to MRI. CT is commonly performed to rule out non-cardiac causes of arrest. Soon after a cerebral ischaemia, energy depletion can lead to cytotoxic oedema. Neuron-specific enolase (NSE) is a marker of neuronal damage and is recommended for prognostication after CA.
During the Targeted Temperature Management After Out-of-Hospital Cardiac Arrest Trial (TTM-trial), researchers described CT findings after CA and also investigated whether generalised oedema alone or in combination with peak-NSE predicted poor outcome. The researchers also investigated the relationship of serum NSE levels to cerebral oedema on head CT.
Neurological outcome was determined at a follow-up approximately 6 months after the cardiac arrest. The Cerebral Performance Category Scale (CPC) was used. Outcome was defined as good cerebral performance (CPC 1); moderate cerebral disability (CPC 2); severe disability (CPC 3); vegetative state (CPC 4); and brain death (CPC 5).
CT examinations in half of the study patients were performed within 24 hours after CA. 79.8% of these were normal and 9.6% were with generalised oedema.
Cerebral oedema was diagnosed in 45.5% of CT examinations performed 24h-7d post-arrest. These patients often had a poor neurological outcome as compared to patients with CT performed before 24h. Within 24h after cardiac arrest, generalised oedema predicted poor outcome with 14.4% sensitivity and 97.6% specificity. In cases where early CT did not show oedema, 58% patients still had poor outcome at 6 months. Generalised oedema on head-CT 24h-7d post-arrest showed 56.5% sensitivity and 100% specificity for predicting poor outcome.
Study researchers also observed that the combination of head CT and peak-NSE improved sensitivity to predict poor outcome as compared to early CT alone.
Overall, the researchers conclude that findings of generalised oedema on non-contrast enhanced head computed tomography, assessed by a local radiologist, is a reliable predictor of poor outcome after cardiac arrest. The presence of genealised oedema can be of great value to guide treatment decisions as well as give early information about expected prognosis. In addition, the combination of head CT with serum NSE-levels further increased the prognostic performance thus providing evidence in favour of multi-modal algorithms.
Source: Resuscitation
Image Credit: JBER
References:
Moseby-Knappe, Marion et al. (2017) Head computed tomography for prognostication of poor outcome in comatose patients after cardiac arrest and targeted temperature management. Resuscitation. doi.org/10.1016/j.resuscitation.2017.06.027
Latest Articles
Head CT for prognostication