The Canadian Agency for Drugs and Technologies in Health has published assessments of monitoring for neuromuscular blockade and for capnography.
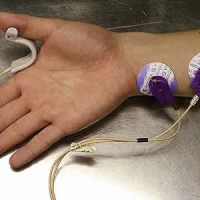
The rapid response report Neuromuscular monitoring for patients receiving continuous paralytic or neuromuscular blocking agents: a review of the clinical effectiveness and guidelinesreviews the clinical efficacy and the evidence-based guidelines on neuromuscular monitoring for guiding treatment and therapy for patients in the intensive care unit (ICU) receiving continuous paralytic or neuromuscular blocking agents (NMBAs).
NMBAs may be used to facilitate short procedures under general anaesthesia, to facilitate mechanical ventilation, to manage patients with increased intracranial pressure, massive haemoptysis, tetanus, or neuroleptic malignant syndrome. The report authors note that evidence for the value of the train of four (TOF) monitoring of patients in ICUs receiving neuromuscular blocking agents (NMBAs) remains unclear. One systematic review, which included three trials comparing TOF monitoring with clinical assessment, reported conflicting results, with benefit being demonstrated with TOF monitoring in one trial and no benefit in two trials. Use of TOF monitoring resulted in lower dose of NMBA being used and a faster recovery of neuromuscular function in one trial but not in two trials. They did not find any relevant evidence-based guidelines.
CPR
Limited evidence was available on the effectiveness of capnography for monitoring adult patients undergoing CPR. For patients experiencing out-of-hospital cardiac arrests, there was evidence for a greater likelihood of return of spontaneous circulation and survival of the acute event for patients monitored with capnography.
In adult patients who needed out-of-hospital CPR, capnography led to improved survival at a higher cost. The incremental cost-effectiveness ratio (ICER) was $27,269 per life saved. The economic findings were found to be highly sensitive to mortality rates. A secondary analysis was conducted using higher survival rates reported in a study from an in-hospital setting, whereby the ICER declined to $4,910 per life saved.
Critically Ill
There was limited evidence to assess the effectiveness of capnography for adult patients in serious or critical condition. The evidence suggested that patients monitored with capnography were less likely to experience an unrecognised misplaced endotracheal tube (ETT) compared with patients who were not monitored with capnography. The interpretation of the results for this population was limited due to a lack of reporting of patient characteristics and details of the intervention and comparator in the two included studies.
For the adult population, it was assumed that the relative treatment effects (incidence of respiratory failure) in the capnography group when compared with standard monitoring would be similar to the relative treatment effect that was observed in adult patients receiving procedural sedation. The exploratory analysis showed that capnography improved survival at a lower cost and was therefore less costly and more effective compared standard monitoring.
The authors recommend research on the impact of capnography on the care continuum for each of the four clinical populations included in the review. They write: “A clearer picture of the clinical decision-making pathway for each population, and comparative evidence in each, could inform a more complete decision-analytic framework and generate more accurate inputs for the economic model. The establishment of levels of severity for hypoxaemia (for example, mild, moderate, severe, and profound), may help to encourage consistent reporting across studies and allow for a more objective assessment of study results. The systematic collection of harms data may help identify patient populations that are particularly susceptible to false alarms or technical problems with the monitoring device.”
The rapid response report Neuromuscular monitoring for patients receiving continuous paralytic or neuromuscular blocking agents: a review of the clinical effectiveness and guidelinesreviews the clinical efficacy and the evidence-based guidelines on neuromuscular monitoring for guiding treatment and therapy for patients in the intensive care unit (ICU) receiving continuous paralytic or neuromuscular blocking agents (NMBAs).
NMBAs may be used to facilitate short procedures under general anaesthesia, to facilitate mechanical ventilation, to manage patients with increased intracranial pressure, massive haemoptysis, tetanus, or neuroleptic malignant syndrome. The report authors note that evidence for the value of the train of four (TOF) monitoring of patients in ICUs receiving neuromuscular blocking agents (NMBAs) remains unclear. One systematic review, which included three trials comparing TOF monitoring with clinical assessment, reported conflicting results, with benefit being demonstrated with TOF monitoring in one trial and no benefit in two trials. Use of TOF monitoring resulted in lower dose of NMBA being used and a faster recovery of neuromuscular function in one trial but not in two trials. They did not find any relevant evidence-based guidelines.
Capnography
While anaesthetists have been using capnography for decades to monitor end-tidal carbon dioxide in patients receiving general anaesthesia, its use outside the operating room, including in the ICU, has been growing. The CADTH’s report assesses the clinical effectiveness and cost-effectiveness of capnography (alone or in combination with other monitoring equipment) in adult and paediatric patients compared with no ETCO2 monitoring, standard monitoring (e.g., pulse oximetry, pulse rate, blood pressure, visual assessment), or other forms of noninvasive respiration and ventilation monitoring in hospital or pre-hospital settings for patients in four categories:- Undergoing procedural sedation,
- Receiving CPR
- In serious or critical condition
- Postoperative patients with known obstructive sleep apnea and/or who are receiving high opioid doses.
CPR
Limited evidence was available on the effectiveness of capnography for monitoring adult patients undergoing CPR. For patients experiencing out-of-hospital cardiac arrests, there was evidence for a greater likelihood of return of spontaneous circulation and survival of the acute event for patients monitored with capnography.
In adult patients who needed out-of-hospital CPR, capnography led to improved survival at a higher cost. The incremental cost-effectiveness ratio (ICER) was $27,269 per life saved. The economic findings were found to be highly sensitive to mortality rates. A secondary analysis was conducted using higher survival rates reported in a study from an in-hospital setting, whereby the ICER declined to $4,910 per life saved.
Critically Ill
There was limited evidence to assess the effectiveness of capnography for adult patients in serious or critical condition. The evidence suggested that patients monitored with capnography were less likely to experience an unrecognised misplaced endotracheal tube (ETT) compared with patients who were not monitored with capnography. The interpretation of the results for this population was limited due to a lack of reporting of patient characteristics and details of the intervention and comparator in the two included studies.
For the adult population, it was assumed that the relative treatment effects (incidence of respiratory failure) in the capnography group when compared with standard monitoring would be similar to the relative treatment effect that was observed in adult patients receiving procedural sedation. The exploratory analysis showed that capnography improved survival at a lower cost and was therefore less costly and more effective compared standard monitoring.
The authors recommend research on the impact of capnography on the care continuum for each of the four clinical populations included in the review. They write: “A clearer picture of the clinical decision-making pathway for each population, and comparative evidence in each, could inform a more complete decision-analytic framework and generate more accurate inputs for the economic model. The establishment of levels of severity for hypoxaemia (for example, mild, moderate, severe, and profound), may help to encourage consistent reporting across studies and allow for a more objective assessment of study results. The systematic collection of harms data may help identify patient populations that are particularly susceptible to false alarms or technical problems with the monitoring device.”
References:
Richardson M, Mouton K, Rabb D et al. (2016) Capnography for
monitoring end-tidal CO2 in hospital and pre-hospital settings. CADTH
health technology assessment; 142. Ottawa: CADTH. March 2016. Available
from https://www.cadth.ca/sites/default/files/pdf/HT0007_End-Tidal_CO2_Review.pdf
Canadian Agency for Drugs and Technologies in Health (2016) Neuromuscular monitoring for patients receiving continuous paralytic or neuromuscular blocking agents: a review of the clinical effectiveness and guidelines. Rapid response report: summary with critical appraisal. 10 Feb. Available from https://www.cadth.ca/sites/default/files/pdf/htis/feb-2016/RC0746-Train%20of%20four-Final.pdf
Canadian Agency for Drugs and Technologies in Health (2016) Neuromuscular monitoring for patients receiving continuous paralytic or neuromuscular blocking agents: a review of the clinical effectiveness and guidelines. Rapid response report: summary with critical appraisal. 10 Feb. Available from https://www.cadth.ca/sites/default/files/pdf/htis/feb-2016/RC0746-Train%20of%20four-Final.pdf
Latest Articles
monitoring, capnography, neuromuscular blockade
The Canadian Agency for Drugs and Technologies in Health has published assessments of neuromuscular blockade and for capnography.