Implementing intermediate care beds in the ICU either physically separate or apart can improve outcomes, said Professor Bertrand Guidet, France, speaking today at the European Society of Intensive Care Medicine congress in Barcelona. ICU patients is like gold in the central bank, defined by illness and not by location.
Guidet acknowledge the starting point of the heterogeneity of icu provision across Europe, in number of ICU beds, their definition, organisation and funding. The European average of ICU beds is 11.5 beds per 100000 capita, but this ranges from 4 up to 30.
Guidet quoted the ESICM Working Group on Quality Improvement’s Recommendations on basic requirements for intensive care units: structural and organisational aspects: “The objectives of an ICU are the monitoring and support of threatened or failing vital functions in criticall ill patients who have illnesses with the potential to endanger life…” the population may present with a large variety of pathologies. This describes intermediate care as well. The ICU is part of the hospital, and ICU physicians have to work outside the ICU, in triage, in the ED. The ESICM recommendations state that “ Timely mobilization of the ICU team and its support services plays an important role in the efficient use of acute care facilities, for the coverage, triage, and outreach management of critically ill patients outside the ICU. Shared protocols between the ICU and other departments of the hospital (e.g., the emergency department) enhance throughput and decrease overall hospital mortality of critically ill patients.”
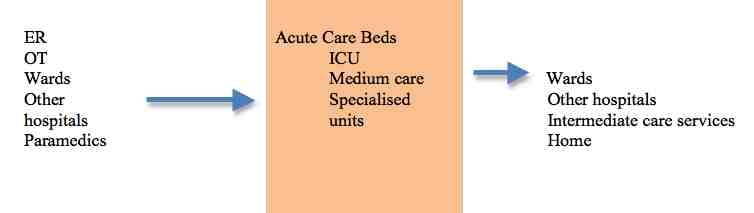
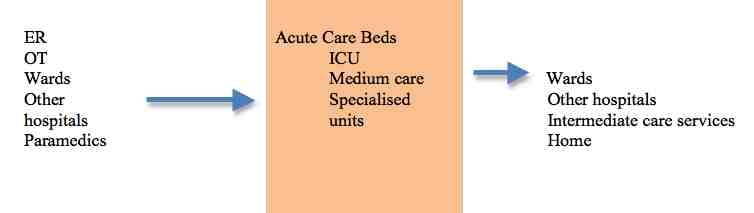
There is a process - input, throughput and output. Acute care beds cover ICU, medium or intermediate care and specialised units, such as coronary care etc.
Nasraway in a paper in Critical Care presented the Guidelines on admission and discharge for adult intermediate care units developed by the American College of Critical Care Medicine, SCCM. These guidelines cover patients that do not require intensive care but need more care than provided on a general ward. It is a cost-effective alternative to critical care unit admission. 20% of beds are occupied by intermediate care patients, i.e. those that do not need organ support.
Stacy in Critical Care Nursing has published the core competencies for nurses working in progressive care units. Nurses working in these units need to be able to perform procedures that are performed in intensive care, so there is a case for using the same nursing team between intermediate care and intensive care. Indeed the American Association of Critical-Care Nurses recognises progressive care as part of the continuum of critical care.
The intermediate care unit serves many patients who will never go to intensive care.
Benefits of Intermediate Care
The potential benefits of having an intermediate care unit include:
There is a way to use illness to define such beds. The workload indexes are NEMS/ TISS/ PRN. The definition by level of care (LOC) would be either I (no organ support) or II (one organ support). No organ support would be intermediate care. The ratio of nurses to patients is 2 FTE per bed or a 1/3 ratio.
Guidet acknowledged the paucity of data regarding the effectiveness, quality of care and safety of intermediate care units. One study is by Peelen et al. in the Netherlands, which looked at severe sepsis. They found that larger annual volume of patients with severe sepsis admitted to Dutch ICUs is associated with lower in-hospital mortality in this patient group. The presence of a MCU as a step-down facility is associated with greater in-hospital mortality.
The ELOISE clinical trial is a multi-centre European observational study to assess whether patients admitted to ICUs with availability of intermediate care units have lower hospital mortality than those admitted to ICUs without availability of intermediate care units. Across Europe the availability is very varied. An article in press in Critical Care will look at these data.
Guidet noted that there are strengths and weaknesses of both models
Separate units
Combined units
Implementing intermediate care has some barriers ; cost constraints, staff shortages, team building and reduction of burnout, and changes in case mix, with more elderly population and patients with several comorbidities.
He concluded that several lines of evidence suggest that intermediate care units should be promoted, but there is a lack of data on efficacy/efficiency and the optimal ratio of ICU/ intermediate care beds. A mixed unit offers several potential advantages in flexibility and use of the same team. However, prospective studies are warranted to prove the benefit of such an organisation.
Patient satisfaction is critical. Patients and families can be distressed if they are transferred to a general ward.
Guidet acknowledge the starting point of the heterogeneity of icu provision across Europe, in number of ICU beds, their definition, organisation and funding. The European average of ICU beds is 11.5 beds per 100000 capita, but this ranges from 4 up to 30.
Guidet quoted the ESICM Working Group on Quality Improvement’s Recommendations on basic requirements for intensive care units: structural and organisational aspects: “The objectives of an ICU are the monitoring and support of threatened or failing vital functions in criticall ill patients who have illnesses with the potential to endanger life…” the population may present with a large variety of pathologies. This describes intermediate care as well. The ICU is part of the hospital, and ICU physicians have to work outside the ICU, in triage, in the ED. The ESICM recommendations state that “ Timely mobilization of the ICU team and its support services plays an important role in the efficient use of acute care facilities, for the coverage, triage, and outreach management of critically ill patients outside the ICU. Shared protocols between the ICU and other departments of the hospital (e.g., the emergency department) enhance throughput and decrease overall hospital mortality of critically ill patients.”
There is a process - input, throughput and output. Acute care beds cover ICU, medium or intermediate care and specialised units, such as coronary care etc.
Nasraway in a paper in Critical Care presented the Guidelines on admission and discharge for adult intermediate care units developed by the American College of Critical Care Medicine, SCCM. These guidelines cover patients that do not require intensive care but need more care than provided on a general ward. It is a cost-effective alternative to critical care unit admission. 20% of beds are occupied by intermediate care patients, i.e. those that do not need organ support.
Stacy in Critical Care Nursing has published the core competencies for nurses working in progressive care units. Nurses working in these units need to be able to perform procedures that are performed in intensive care, so there is a case for using the same nursing team between intermediate care and intensive care. Indeed the American Association of Critical-Care Nurses recognises progressive care as part of the continuum of critical care.
The intermediate care unit serves many patients who will never go to intensive care.
Benefits of Intermediate Care
The potential benefits of having an intermediate care unit include:
- greater flexibility in patient triage
- increase accessibility to limited critical care
- cost-effective alternative to ICU admission
- promote faster recovery
- support timely discharge from the ICU
- reduce ICU readmission (“bouncebacks”)
- increase pat satisfaction - reduction of noise, liberal family visitation
There is a way to use illness to define such beds. The workload indexes are NEMS/ TISS/ PRN. The definition by level of care (LOC) would be either I (no organ support) or II (one organ support). No organ support would be intermediate care. The ratio of nurses to patients is 2 FTE per bed or a 1/3 ratio.
Guidet acknowledged the paucity of data regarding the effectiveness, quality of care and safety of intermediate care units. One study is by Peelen et al. in the Netherlands, which looked at severe sepsis. They found that larger annual volume of patients with severe sepsis admitted to Dutch ICUs is associated with lower in-hospital mortality in this patient group. The presence of a MCU as a step-down facility is associated with greater in-hospital mortality.
The ELOISE clinical trial is a multi-centre European observational study to assess whether patients admitted to ICUs with availability of intermediate care units have lower hospital mortality than those admitted to ICUs without availability of intermediate care units. Across Europe the availability is very varied. An article in press in Critical Care will look at these data.
Guidet noted that there are strengths and weaknesses of both models
Separate units
- step down facility
- noise reduction
- less nosocomial infection
- family visits
Combined units
- flexibility
- discharge/readmission
- team building
- handover
- continuity of care
- shared responsibility
Implementing intermediate care has some barriers ; cost constraints, staff shortages, team building and reduction of burnout, and changes in case mix, with more elderly population and patients with several comorbidities.
He concluded that several lines of evidence suggest that intermediate care units should be promoted, but there is a lack of data on efficacy/efficiency and the optimal ratio of ICU/ intermediate care beds. A mixed unit offers several potential advantages in flexibility and use of the same team. However, prospective studies are warranted to prove the benefit of such an organisation.
Patient satisfaction is critical. Patients and families can be distressed if they are transferred to a general ward.
Latest Articles
ESICM 2014, Intermediate Care
Implementing intermediate care beds in the ICU either physically separate or apart can improve outcomes, said Professor Bertrand Guidet, France, speaking t...










