ICU Management & Practice, Volume 23 - Issue 1, 2023
Introduction
Catalonia is one of the autonomous communities of northern Spain. It has a surface area of 32,114 m2 and a population of 7,747,709 inhabitants. The Emergency Medical System (known in Spanish as the Sistema de Emergencias Médicas, SEM) is part of CatSalut, the Catalan Health Service, and is the public entity that provides support services for medical emergencies in the region. As of 1995, it has two advanced life support ground units that are specialised in paediatric and neonatal transport, located at the Vall d'Hebron University Hospital and the Sant Joan de Déu University Hospital, which operate 24 hours a day, 365 days a year. It also has a specialised paediatric and neonatal aerial unit that is operated by personnel from the Parc Taulí and Santa Creu i Sant Pau university hospitals in Sabadell and Barcelona respectively, plus a nurse paediatric basic life support unit during the winter months. The team is composed of more than 60 professionals, including paediatricians and nurses with training in paediatric and neonatal care and medical emergency technicians specialised in paediatrics.
Since the creation of the paediatric SEM, more than 30,000 children have been transferred, among which approximately 40% were neonates. Around 95% of the activity corresponds to interhospital transfers, involving the stabilisation and transfer of critically ill or injured children to receiving hospitals that can handle their level of complexity. As of several years ago, these teams also respond to incidents in homes, public areas, and primary care centres when they are required to accompany the regional intermediate or advanced life support units. Since 2019, these units can also transfer critically ill patients who are connected to ECMO devices.
The paediatric SEM's activity is managed from the SEM coordination centre, who receives the request for patient transfer, coordinates the transfer to the appropriate hospital centre, and assigns the proper health transport resource.
The Paediatrician as Part of the SEM Coordination Centre
Up to 2017, the activity of the paediatric SEM was managed by SEM professionals from the coordination centre who were not specialised in paediatrics. That year, the SEM Health Coordination Centre began having a paediatric physician on call 24 hours a day, 365 days a year. Since then, that role has become key for coordinating resources, providing both telephone support for healthcare teams in the region and guidance in paediatric emergencies.
This task is carried out by the same paediatricians who are part of the aforementioned paediatric advanced life support units. Thus, they are knowledgeable not only about serious medical conditions, but also about the particularities of initial medical attention outside of health centres and transport. This new facet of their work has been a challenge for these professionals, who up to then had provided only on-site medical support.
Tasks of the Paediatrician in the Coordination Centre
1. Managing interhospital transfers: coordination and assessment
Initially, they directly managed the transfers for patients ≤ 6 years of age and provided support for the interhospital transfer team for patients > 6 years of age. They now currently manage transfers for patients
< 16 years of age.
When a call comes in from a health centre for the transfer of a paediatric or neonatal patient, it will firstly be routed to a call centre operator who will request the basic information needed. Next, it will be immediately transferred to the coordinating paediatrician, who will evaluate the patient's situation, assess the possible additional treatment measures, and decide on the most appropriate destination centre and transportation resource. It is worth noting that the transport may not always be performed by a paediatric unit, depending on the availability, coordination, and time dependence of the medical condition.
2. Telephone support for emergencies
The other function of the coordinating paediatrician is to provide support for consultations that may require specialised care due to their complexity and severity. These may be:
- Calls made by citizens which have first been screened by professional call managers (non-paediatric physicians or nurses). These are usually calls flagged by the system as high priority (Priority 0), where the reason for the call is a serious situation, such as unconsciousness, severe breathing difficulty, and/or other life-threatening circumstances.
- Consultations from SEM healthcare teams caring for paediatric patients or other professionals from healthcare centres.
In all of these cases, we collaborate with other members of the coordination centre to send, if necessary, the proper resource as determined by the evaluation made.
How the Paediatrician Collaborates From the Coordination Centre in Paediatric and Neonatal Emergencies
The fact that paediatricians with specific training in paediatric and neonatal emergencies and critical care can remotely assess the initial stabilisation of these patients provides an additional point of support from the healthcare system. In the execution of these tasks, the information transferred is the fundamental element.
With respect to the information on the patient's clinical situation, some basic, structured information on the physical examination and vital signs is requested, in addition to that regarding the treatments and additional diagnostic tests already performed. This information is used to evaluate the situation and enable the professionals to suggest additional measures (whether treatment-related or diagnostic), if any are needed. If, due to the patient's condition, the coordinating paediatrician decides to immediately send one of the paediatric ground units, they will alert the sending centre and offer them guidance. The ground unit will then also contact the sending centre directly to determine the patient's situation and be able to suggest measures that will continue following their arrival.
This bi-directional and regulated communication in emergency situations will always be systematic (following the ABCDE sequence), concise, objective (using scores, particular vital signs, etc.), specific (i.e. specifying the units of the analytical parameters), and cross-checked when sensitive information is being sent (meaning that it should be repeated by the other person to ensure that the information was correctly understood, i.e. for a dose of medication).
Later, if the patient does indeed need to be transferred, the proper healthcare resource will be chosen after carefully considering different factors. These factors are mainly:
- Clinical condition of the patient and their current and/or foreseeable needs: For example, a stable patient for whom advanced lifesaving measures are not foreseen to be needed in the next few hours can be transferred by conventional means (transport technicians); this also applies to term neonates who present good thermoregulation and whose weight is > 2.5 kg.
- Availability of resources: It should be kept in mind that the paediatric units cover all of Catalonia and Andorra. If the units are busy or response times are very long, it will be necessary to propose to the centre sending the patient that a non-paediatric transport unit be used, justifying the reason for this.
- Time dependence: When faced with certain medical conditions for which it is completely impossible for the centre of origin to offer the treatment needed, the fastest resource should be chosen, as long as it is possible to ensure the stabilisation of the patient prior to and during the transport.
Lastly, the coordinating paediatrician will select the receiving centre according to the needs they feel that patient has, taking into consideration the information given and the availability of each centre. If possible, they will also consider the preferences of the centre of origin and how close the family lives. For some medical conditions, the distribution guidelines established by CatSalut will be followed.
How Much Activity Have the Paediatricians at the Coordination Centre Had Since 2017?
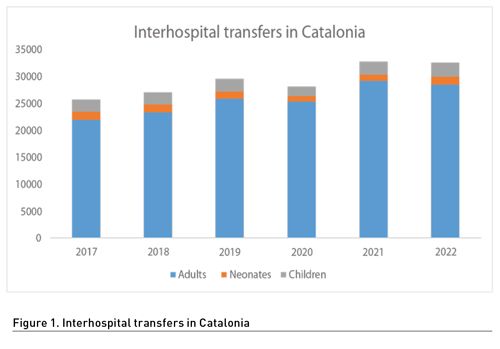
Since 2017, when these paediatricians started to work at the coordination centre, more than 175,956 interhospital transfers have been handled, of which 7,806 were neonatal transfers and 16,469 were paediatric transfers (4.4% and 9.35% of the total transfers, respectively). Managing transfers for paediatric patients has been done by the coordinating paediatrician, along with the professionals who were in charge of this function before 2017 (non-paediatric physicians and nurses). The most frequent reasons for transfer were respiratory pathologies, infectious pathologies, and being born premature. Figure 1 shows the transfers per year and in it we can observe a decrease in paediatric activity that coincides with the SARS-CoV-2 pandemic. Less paediatric pathologies were recorded during this time, a phenomenon which is already well known.
As regards telephone support for paediatric consultations, between 2017 and 2021 more than 642,761 calls were taken. Of these, 25,775 (4%) were flagged as Priority 0. They were sent to the coordinating paediatrician and the other consultation, medical, and nursing professionals.
Future Challenges
The SEM, in collaboration with the paediatric units, has identified several challenges in its efforts to provide more efficient patient care and management and adapt to the new needs of the system.
- Protocolisation of the management of calls flagged as Priority 0, to avoid both the coordinating paediatrician having to take non-emergency calls and them not receiving these emergency calls at all.
- Direct participation in the paediatric palliative care network, helping to cover its transfer needs.
- Definitively establishing a telemedicine programme using a videoconferencing platform to be able to evaluate patients with the aid of real-time images.
- Better guidance for the centres sending patients and better management of the distribution of patients requiring transport, with full information on the resources available at each centre for paediatric or neonatal care.
- Homogenisation of the initial support, regardless of the patient's location in the region.
Conclusion
The role of the paediatrician at the coordination centre is becoming increasingly important within the SEM as a professional specialised in paediatric and neonatal critical care. These physicians not only assess the initial stabilisation of this kind of patient, whether at a private home or at healthcare centres, they also play an essential role in managing the resources of the Catalan healthcare system, as regards both transportation units and the centres receiving patients. Overall, the general opinion of these last 5 years is very positive, with the service being well-perceived by the professionals using it. The fact that the coordinating paediatricians are the same professionals that work in the specialised advanced support units has improved territorial equality in patient care and fostered a model focused on the child and their family.
Conflict of Interest
None.















