ICU Management & Practice, Volume 18 - Issue 3, 2018
Fibrinogen replacement
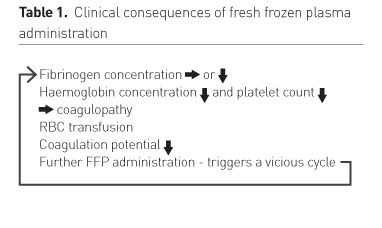
Fresh frozen plasma
Fibrinogen replacement therapy
Fibrinogen concentration measurement
Tranexamic acid
Prothrombin complex concentrate
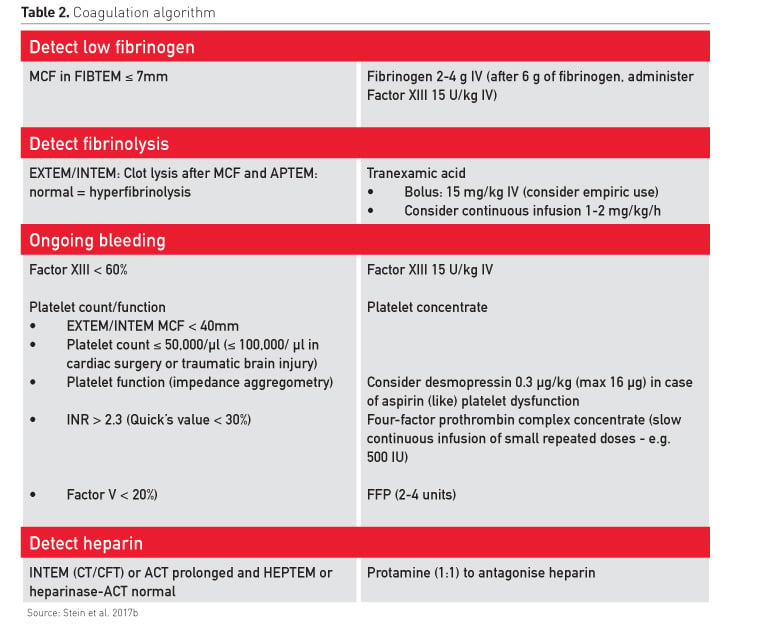
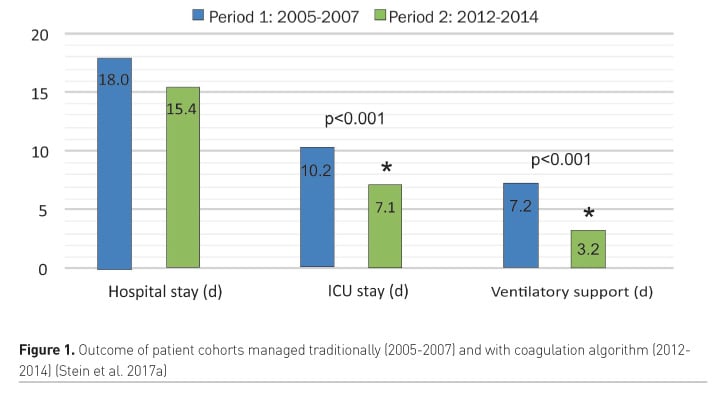
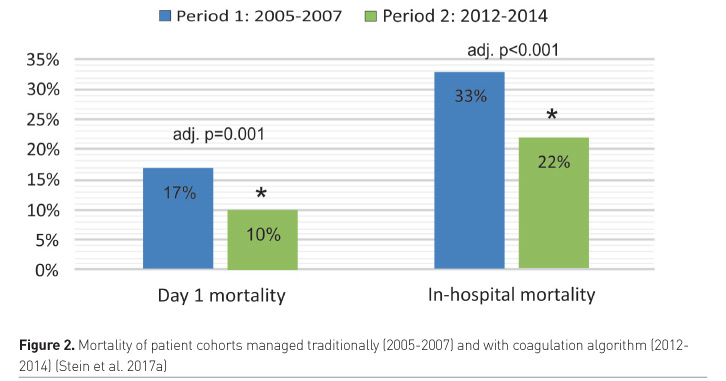
Coagulation algorithm
Key Points
- Fibrinogen is the coagulation element that becomes critically reduced first in many instances
- In trauma and cardiac surgery patients, the critical level is 1.5 to 2.0 g/L
- Immediate viscoelastic coagulation monitoring is key for individualised goal-directed coagulation algorithms
- Coagulation algorithms should be available in every hospital
- Compliance with the European trauma treatment guidelines improves survival
Abbreviations
FFP fresh frozen plasma
MCF maximum clot firmness
PCC prothrombin complex concentrate
RBC red blood cells
ROTEM rotational thromboelastometry
TEG thromboelastography
References:
Eder AF, Herron R, Strupp A et al. (2007) Transfusion-related acute lung injury surveillance (2003-2005) and the potential impact of the selective use of plasma from male donors in the American Red Cross. Transfusion, 47(4): 599-607.
Garrigue D, Godier A, Glacet A et al. (2018) French lyophilized plasma versus fresh frozen plasma for the initial management of trauma-induced coagulopathy: a randomized open-label trial. J Thromb Haemost, 16(3): 481-9.
Goldstein JN, Refaai MA, Milling TJ Jr et al. (2015) Four-factor prothrombin complex concentrate versus plasma for rapid vitamin K antagonist reversal in patients needing urgent surgical or invasive interventions: a phase 3b, open-label, non-inferiority, randomised trial. Lancet, 385(9982): 2077-87.
Grassin-Delyle S, Theusinger OM, Albrecht R et al. (2018) Optimisation of the dosage of tranexamic acid in trauma patients with population pharmacokinetic analysis. Anaesthesia, 73(6): 719-29.
Holcomb JB, Tilley BC, Baraniuk S et al.; PROPPR Study Group (2015) Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA, 313(5): 471-82.
Innerhofer P, Fries D, Mittermayr M et al. (2017) Reversal of trauma-induced coagulopathy using first-line coagulation factor concentrates or fresh frozen plasma (RETIC): a single-centre, parallel-group, open-label, randomised trial. Lancet Haematol, 4(6): e258-e271.
Levy JH, Goodnough LT (2015) How I use fibrinogen replacement therapy in acquired bleeding. Blood, 125(9): 1387-93.
Maegele M (2010) Acute traumatic coagulopathy: Incidence, risk stratification and therapeutic options. World J Emerg Med, 1(1): 12-21.
Mannucci PM (2004) Treatment of von Willebrand’s disease. N Engl J Med, 351: 683-94.
Monroe DM, Roberts HR, Hoffman M (1994) Platelet procoagulant complex assembly in a tissue factor-initiated system. Br J Haematol, 88(2): 364-71.
Nascimento B, Callum J, Tien H, et al. (2013) Effect of a fixed-ratio (1:1:1) transfusion protocol versus laboratory-results-guided transfusion in patients with severe trauma: a randomized feasibility trial. CMAJ, 185(12): E583-9.
National Institute for Biological Standards and Control (2008) World Health Organization
1st international standard for fibrinogen concentrate. [Accessed: 29 June 2018] Available from nibsc.org/documents/ifu/98-614.pdf
Rana R, Fernández-Pérez ER, Khan SA et al. (2006) Transfusion-related acute lung injury and pulmonary edema in critically ill patients: a retrospective study. Transfusion, 46(9): 1478-83.
Rossaint R, Bouillon B, Cerny V et al. (2016) The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care, 20: 100.
Sarani B, Dunkman WJ, Dean L et al. (2008) Transfusion of fresh frozen plasma in critically ill surgical patients is associated with an increased risk of infection. Crit Care Med, 36(4): 1114-8.
Schlimp CJ, Ponschab M, Voelckel W et al. (2016) Fibrinogen levels in trauma patients during the first seven days after fibrinogen concentrate therapy: a retrospective study. Scand J Trauma Resusc Emerg Med, 24: 29.
Silliman CC, Ambruso DR, Boshkov LK (2005) Transfusion-related acute lung injury. Blood, 105(6): 2266-73.
Solomon C, Baryshnikova E, Tripodi A et al. (2014) Fibrinogen measurement in cardiac surgery with cardiopulmonary bypass: analysis of repeatability and agreement of Clauss method within and between six different laboratories. Thromb Haemost, 112(1): 109-17.
Spahn DR, Asmis LM (2009) Excessive perioperative bleeding: are fibrin monomers and factor XIII the missing link? Anesthesiology, 110(2): 212-3.
Stanworth SJ, Brunskill SJ, Hyde CJ et al. (2004) Is fresh frozen plasma clinically effective? A systematic review of randomized controlled trials.
Br J Haematol, 126(1): 139-52.
Stein P, Kaserer A, Sprengel K et al. (2017a) Change of transfusion and treatment paradigm in major trauma patients. Anaesthesia, 72(11): 1317-26.
Stein P, Kaserer A, Spahn GH et al. (2017b) Point-of-care coagulation monitoring in trauma patients. Semin Thromb Hemost, 43(4): 367-74.
Stein P, Studt JD, Albrecht R et al. (2018) The Impact of Prehospital Tranexamic Acid on Blood Coagulation in Trauma Patients. Anesth Analg, 126(2): 522-9.
Theusinger OM, Goslings D, Studt JD et al. (2017) Quarantine versus pathogen-reduced plasma-coagulation factor content and rotational thromboelastometry coagulation. Transfusion, 57(3): 637-45.
Watson GA, Sperry JL, Rosengart MR et al. (2009) Fresh frozen plasma is independently associated with a higher risk of multiple organ failure and acute respiratory distress syndrome. J Trauma, 67(2): 221-7.
Weber CF, Görlinger K, Meininger D et al. (2012) Point-of-care testing: a prospective, randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Anesthesiology, 117(3): 531-47.
Welsby IJ, Troughton M, Phillips-Bute B et al. (2010) The relationship of plasma transfusion from female and male donors with outcome after cardiac surgery. J Thorac Cardiovasc Surg, 140(6): 1353-60.
Whiting P, Al M, Westwood M, et al. (2015) Viscoelastic point-of-care testing to assist with the diagnosis, management and monitoring of haemostasis: a systematic review and cost-effectiveness analysis. Health Technol Assess, 19(58): 1-228.








