ICU Management & Practice, Volume 22 - Issue 1, 2022
Paediatric and maternity hospitals report far fewer deaths each year than adult general hospitals. Nevertheless, each case of death in these hospitals should not be less deserving of being analysed by the mortality review committee (MRC). In this way, by analysing each case and seeking strategies for improvement, the quality of care for other patients who may find themselves or end up in a similar situation can be optimised.
In addition, the MRC is a multidisciplinary tool that allows the end-of-life situations of different specialties to be compared, thus also enabling mutual learning on how to deal with them in difficult periods of life such as childhood, adolescence or pregnancy.
Barcelona Children's Hospital SJD is a highly specialised university centre for the treatment of children and pregnant women. It is a private, non-profit institution that is dedicated to public service since its creation in 1867 and belongs to the Hospitaller Order of Saint John of God, which manages more than 300 healthcare centres in 50 countries around the world and serves the most vulnerable groups in hospitals, health centres and social services. More than 2,100 professionals work at the hospital and it counts with more than 500 volunteers, 314 beds, 161 consulting rooms and more than 50 hospitalisations and 335 emergencies per day according to the annual report of 2019. In our case, the MRC is regulated by the Spanish National Institute for Health.
Purpose of the Mortality Review Committee
Its objective is to contribute to the improvement of the quality of care by evaluating and analysing in-hospital mortality and channelling the improvement actions proposed as a result of this analysis. MRC brings together experts who guarantee that the actions take into account different points of view, experiences, knowledge and skills, and those are produced in a harmonious and synchronised way within the hospital.
We analyse clinical management, processes, teamwork and especially holistic aspects. The perinatal mortality and the death of a child is always a devastating process for the family. The MRC also reviews whether the families have received all the support they need and that our hospital can provide. It also monitors the impact of deaths on our staff to check the special needs of our teams. We perform an annual report of the activity in this committee and register the trends on mortality in our hospital, as well as other quality indicators related to mortality. Another purpose of this committee is to increase the performance of autopsies in our hospital.
The MRC Team
The MRC is a multidisciplinary committee articulated by a chairperson and a secretary. The chair is responsible for leading the meeting and coordinating the entire team. The secretary is responsible for scheduling the meeting and setting the agenda, as well as taking the minutes during the meeting and updating all the information and data collected from the meetings.
The departments represented on the mortality committee should be all those that are primarily responsible for patients who have died or may die in the hospital (cardiology, neurology, chronic and palliative care, oncology, haematology, paediatric surgery, gynaecology and obstetrics, as well as emergency, paediatric hospitalisation, neonatal and paediatric intensive care). These departments are mostly represented by physicians, although some of them also have nursing representation. The presence of nurses has been promoted, due to their crucial role in patient care and giving support to their families. In addition, as our centre is a hospital where specialised healthcare training takes place, residents in training are also invited to participate. Another department represented on the committee is the anatomical pathology department whose vision complements and helps to understand the outcome of the cases analysed and provides further information regarding the cases with a post-mortem examination. The MRC is also a competence of the quality and medical directors, so they are also active members of this committee. Their commitment underlines the importance of this group.
In these meetings there is an atmosphere of trust, with kindness by all members. Detailed analysis is facilitated in a psychologically safe environment, which is essential for admitting incidents and finding changes and opportunities for improvement.
MRC Meetings - Periodicity and Duration
The mortality committee meets on a monthly basis, although exceptionally there may be two meetings in a month if there are many cases or other issues to discuss at the meeting. The usual duration of the meetings is between one to two hours.
Prior to the MRC, each department discusses relevant cases with the rest of its team. Infant, fetal and maternal death closure meetings are held periodically in the hospital departments participating in the MRC. Following these meetings, the department representative on the MRC makes a report that is reviewed and discussed at the monthly MRC meeting.
This methodology has two main advantages: first, it speeds up MRC meetings and makes them more efficient. Secondly, the analysis of each team is crucial for the MRC members. Most of the time, the representative brings the observed weaknesses and proposed improvement actions. These are critically analysed by the committee in a constructive model to provide the best experience for the teams and the best in excellence for the whole institution.
MRC Meetings – Points of Discussion
Throughout each meeting, different cases of death are presented and discussed, most of them in first review and some in second review, proposals for improvement are established, proposals from previous meetings are reviewed and other issues are discussed.
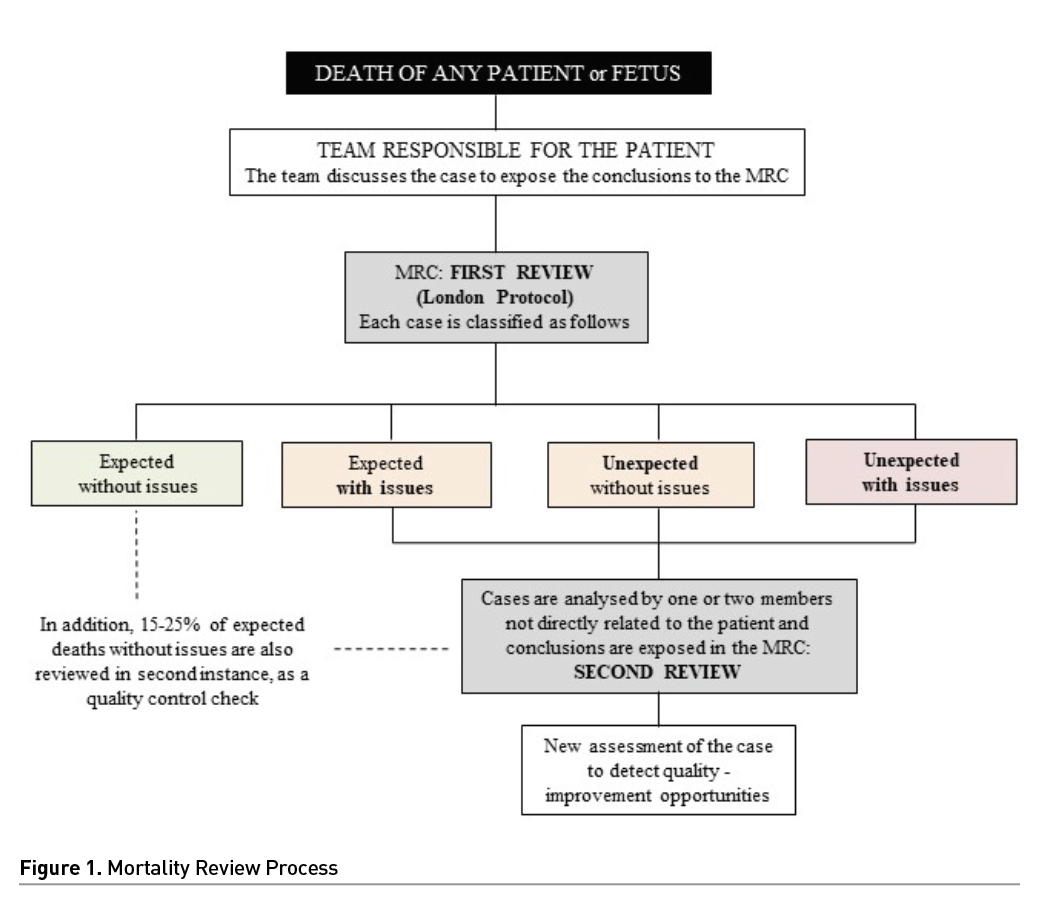
The London protocol root cause analysis is the mortality-review process used. This protocol identifies care delivery processes and any contributory factors. MRC members label each case as death expected or unexpected (if it was not foreseeable at the time of admission or throughout the hospital stay) and without or with issues (with quality-improvement opportunity). This classification must be validated by all the members of the committee (Figure 1).
As an example of our activity, in 2020 we analysed 83 exitus in the MRC, which represents 0.49% of 16737 admissions. The percentage of unexpected deaths was 9.63% (8/83) and deaths with issues, 6.02% (6/83). The intraoperative mortality was 0.007% (1/13881 surgeries). Autopsies were performed in 77.1% of deaths (64/83).
First reviews
In each meeting, a first review of all cases of death from the previous month are presented, as well as each one of the actions that were carried out by the medical team. Cases are exposed by the last team responsible for the patients. As we have mentioned before, these cases have been previously analysed by the primary teams.
The MRC members present at the meeting discuss and debate the management of the case and other related aspects. All members have the opportunity to give their opinion and the actions are validated by the whole committee. Each case is classified as follows: death to be expected or not, and death with or without issues. Improvement actions that could be applied to other similar patients are proposed. A person or team responsible for the actions is appointed.
Second reviews
Second case reviews are basically performed in two circumstances: in those cases where death was expected but issues were found and in those where death was not expected. Unlike the first review, which is presented to the mortality committee by the last team responsible for the patient, the second review is performed by one or two teams not directly related to the patient and who are members of the MRC. This member will again review the entire episode (and if necessary, the rest of the patient's medical record) to reissue a new assessment of the case and detect additional points of improvement from a more external point of view. It is advisable that the team that presented the case for the first time be present at the presentation of the second review, to discuss if any points are needed on the analysis made. These second reviews are very productive and beneficial for the teams and the MRC. In addition, 15-25% of expected deaths previously categorised as without issues are randomly reviewed and are also reviewed in a second instance, as a quality control tool. In 2020, we performed 16 second reviews out of 83 exitus (19.3%).
Follow up of improvement actions
Following every review (either first or second), improvements to the case may be proposed by any member of the MRC. Improvements suggested may be diagnostic and therapeutic, logistical or otherwise. The proposals made will be discussed in the committee and, if it is believed that they would have led to a better outcome of the case (not necessarily to avoid death), their implementation will be assessed in order to improve the quality of care offered by the centre to other patients who may be or may end up in similar circumstances. It is important that, at the organisational level, for each proposal made, it is decided which actions will be carried out, who will be responsible to implement them and when it will be reviewed again by the committee.
In fact, the status of improvement actions will also be discussed in future meetings. In 2020, 19 improvement actions were proposed, of which 13 (68.4%) were closed in 2020 and 6 (31.6%) were developed in 2021. Some of these improvement actions were: complete revision of the necrotising enterocolitis protocol, prevention of abdominal compartment syndrome in patients with congenital diaphragmatic hernia, revision of obstetrics protocols (maternal syphilis, chorioamnionitis), sepsis detection protocol and specific course for all hospital staff, creation of a team responsible for accompanying families after a death, among others.
Other topics
In addition to presenting case reviews and discussing improvement actions, every MRC meeting should have an open space at the end to discuss other topics that may be of interest to the committee. Examples of this could be literature reviews on a relevant topic related to hospital mortality, presentation of improvement projects presented in other centres to assess their feasibility on our own, as well as any other topic that a member of the committee believes may be of interest. In addition, this space can be used to discuss issues that cut across the centre's ethics and mortality committees (e.g. organ donation in paediatrics).
Last but not least positive actions detected during the case review (as well as processes, or management) are also assessed. It is based on Hollnagel's safety model (Hollnagel 2014). According to Hollnagel, the preoccupation with the traditional primary focus on error and risks (Safety 1) often leads to undervaluing an equally important safety force, namely inherent human resilience and preventive measures (Safety 2), by understanding the things that go right in everyday work. Fostering an appreciation of Safety 1 and 2 is the key to creating the greatest impact on quality, efficiency and patient safety.
Future Expectations
It is true that there is more and more knowledge about how to deal with end-of-life situations and less and less social taboo about death. Even so, deaths in paediatrics and obstetrics, both because of their infrequency and, in some cases, their unexpectedness, are still an issue that needs further work.
On the other hand, the development and optimisation of new diagnostic and therapeutic techniques in all specialties leads to the appearance of new clinical scenarios on a permanent basis, which means that the teams in charge of these patients must be aware of and actively debate the limitation/adequacy of the therapeutic effort and the decisions regarding the end of life of the patients for whom they are responsible. The subsequent review of deaths, especially in these new scenarios, allows a critical spirit to be maintained and to analyse what has been done correctly and what can be improved for similar situations.
Moreover, certain ethical debates, such as euthanasia or abortion, both regulated nowadays in our country, open the door to new scenarios that will surely be the subject of analysis by the hospital's ethics committee and, probably in some cases, also by the MRC. In this line of ethical debates, asystolic organ donation in paediatrics will also be an issue to be addressed in the coming years. In addition, new scenarios such as the possibility of extubation at home in case of end-of-life situations in terminally ill patients should be considered in our committee.
Another future challenge for the mortality committee is to analyse and try to establish lines of improvement in the face of the exponential increase in cases of suicide and suicide attempts among the paediatric and juvenile population, especially following the start of the pandemic in March 2020.
Conclusions
The perinatal and paediatric mortality committee is a relatively simple tool to apply and carry out, allowing improvements to be implemented both at department level (through the review that each team carries out of its cases before presenting them to the committee) and at hospital level (once they are presented to the MRC). Beyond the cases presented, the relevance of the mortality committee lies above all in the strategies for improvement that are put forward at the meetings. Moreover, being a multidisciplinary committee allows for mutual learning between the different departments of the hospital.
Due to the continuous progress inherent in science, as well as constant social changes, we will inevitably encounter new situations every day that will make us rethink what we have learnt so far. In this constant change of paradigms, the mortality committee is a necessary entity as a quality strategy for the hospital, due to its constant self-analysis and search for improvement in the quality of care for our patients.
Conflict of Interest
None.
References:
BoletínOficial del Estado (1987) Real Decreto 521/1987, de 15 de abril, por el que se aprueba el ReglamentosobreEstructura, Organización y Funcionamiento de los Hospitalesgestionados por el Instituto Nacional de la Salud. Boe. 1–14.
Department of Health and Social Care and Department for Education (2018) Child Death Review Statutory and Operational Guidance (England). Available at https://www.gov.uk/government/publications/child-death-review-statutory-and-operational-guidance-england
Hollnagel E (2014) Safety-I and safety-II: The past and future of safety management.CRC Press.
Magnus DS, Schindler MB, Marlow RD, Fraser JI (2018) A Service evaluation of a hospital child death review process to elucidate understanding of contributory factors to child mortality and inform practice in the English National Health Service. BMJ Open. 8(3):e015802.
Romaguera A, Angels M, Xavier C et al. (2006). Análisis de la mortalidadcomoherramienta de mejora de la calidadasistencialen un servicio de cirugía general. Cirugia Espanola. 80. 78-82.
Tiwari D, O'Donnell A, Renaut R et al. (2020) Reducing hospital mortality: Incremental change informed by structured mortality review is effective. Future Healthc J.(2):143-148.
Willcox ML, Price J, Scott S et al. (2020) Death audits and reviews for reducing maternal, perinatal and child mortality. Cochrane Database Syst Rev. 3(3):CD012982.









