ICU Management & Practice, Volume 22 - Issue 1, 2022
Introduction
Medicines are the most widely used intervention in the critical care environment, and errors in medication use are a well-established complication. Medication errors have been broadly defined as any error in the prescribing, dispensing, or administration of a drug. Unlike adverse drug events which may be unpreventable, medication errors are considered preventable and may or may not have the potential to cause patient harm (Leape and Berwick 2005).
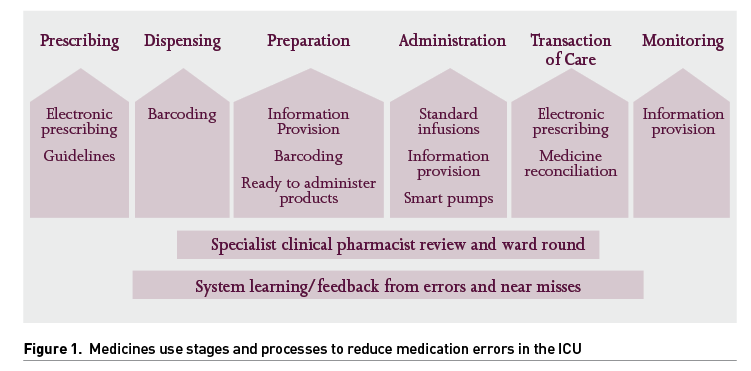
In general, medication errors occur at various stages of the medication management process as described in Figure 1 (Elliott et al. 2021). This review will focus on the prevalence and impact of these types of error in the ICU and assess the processes that are designed to reduce the incidence.
Considering the nature of critical care, where patients require acute treatment often with multiple injectable medicines, it is unsurprising that medication errors are the commonest type of medical error encountered, accounting for 78% of serious medical errors (Rothschild et al. 2005). Most errors originate in the administration phase (Latif et al. 2013). A study of parenteral medication administration errors conducted over 24 hours in 113 intensive care units across 27 countries found that errors occurred at a rate of 74.5 events per 100 patient days (Valentin et al. 2009).
In the United Kingdom (UK), incidents involving medicines were the third largest group (nine percent) of all incidents reported to the national reporting and learning system. A detailed analysis of 72,482 medication incidents found the 100 most serious medication incident reports of death and severe harm were caused by errors in medicine administration (41%), followed by prescribing (32%). Of note, incidents involving injectable medicines represented 62% of all reported incidents leading to death or severe harm (Cousins 2007).
It is important to identify the stages at which the errors occur and the causative and contributory factors to develop preventative strategies and interventions. Many factors have been identified, including inadequate written communication (prescriptions, documentation, transcription), problems with medicines supply and storage, high perceived workload and patient acuity (Keers et al. 2013).
Prescribing
Instituting electronic prescribing (EP) in the ICU has had a profound effect on reducing medications errors. Many of the hospital-wide EP systems are not suitable for ICU use as they are not sophisticated enough to manage the continuous infusions that are commonly used. However these hospital-wide systems do have some excellent functionality e.g. allergy and drug interaction alerts, which many specific ICU systems lack. Many ICUs use the EP component of ICU clinical information management systems, without the basic functionality that is expected. There are now several electronic health records systems (EHRS) that include prescribing, notes and charting throughout the hospital. Whilst these may lack some of the functionality of a specific ICU system, they do benefit from the significant infrastructure underpinning the platform. A single hospital-wide EHRS eliminates transcription errors of prescribing when patients move in and out of ICUs.
In general, introduction of ICU EP system have led to a reduction in the medication error rate compared to hand-written charts (Shulman et al. 2005). But the types of error change with EP, leading to the introduction of new types of error which can be more serious than those seen with paper. EP does eliminate errors due to poor handwriting, abbreviations, non-approved drug names etc. It also provides decision support via the use of pre-written templates which can be set up to include key information that address common questions or scenarios and ‘nudge’ practice to approved pathways. This improves the consistency of prescribing and provides a means to control prescribing and administration practice throughout the day.
However the use of a stand-alone ICU system within a hospital produces significant problems of integration into the wider hospitals systems. Ward staff may be unable to access the ICU system and as such are ‘locked out’ by the technology, at odds from the concept of ‘critical care without walls’.
Overall, the EP systems are beneficial but there are significant limitations which should be acknowledged and addressed by software manufacturers.
Systems that include decision support may add an additional layer of safety but there is an issue of ‘alert fatigue’ (Kane-Gill 2018). Work is ongoing to improve the specificity of alerts and machine learning (Syed et al. 2021) may help, as this field develops.
Specialist clinical pharmacists identify many prescribing errors in the course of their daily drug chart review. Their role is discussed further towards the end of this article. Pharmacist review is important is identifying prescribing errors. Decision support within EHRS system can prevent unintended overdoses and guide dosing, but these systems can be circumvented by prescribers. Similarly, dosing needs to be optimised to the individual patient’s requirements, which is beyond the capability of current systems and needs a specialist pharmacist to augment.
‘Closed-unit’ Prescribing in the ICU
ICUs are unusual within a hospital as the unit takes over the primary care of the patient once their healthcare needs cannot be met on a general or specialist ward. The primary team are no longer responsible for the day-to-day care of the patient, but their expertise is relied upon to advise on the specialist aspects of care. However the specialist practice may be at odds with ICU practice for example with regard to anti-infective length of course, dosing, or indeed initiation and deprescribing. Communication and collaboration is important between the teams, but some units do not allow the primary team to prescribe on the ICU. Running a ‘closed unit’ in this way, maintains an important principle that necessitates bedside communication as a requisite for changing the drug chart. In the absence of this, other teams can prescribe on the ICU without communication, and this may go against the overriding plans and unit guidelines. This lack of rigour can lead to medications errors, as the ICU may not fully understand the plan. This area of practice has not been researched but is a practical area which may impact on medications errors. An obvious exception to this will be the specialist prescribing of chemotherapy on the ICU. Here the ICU doctors do not have the necessary knowledge and competency to perform this safely.
Dispensing
These errors can occur in pharmacy but more commonly are related to ‘picking’ errors in the ICU. Most medications are supplied as stock in the ICU and there is a potential to select the wrong medication. The intervention aimed at reducing this is ‘double-checking’ with another co-worker before administration. This time consuming activity appears to detect some types of errors more than others (Douglass et al. 2018), in some cases the second checker may dissuade the first nurse from acting on the error!
An example of an ICU specific ‘picking error’ is the recurrently noted error of inadvertently hanging a glucose-containing infusion bag instead of saline for arterial line flushing. This can lead to misinterpretation of an apparent hyperglycaemia, leading to prescribing insulin therapy, causing a potentially dangerous hypoglycaemic episode (Gupta and Cook 2013). This error occurs despite the many systems in place and would benefit from an industry-led approach to ‘engineer-out’ this practice by having unique connectors between the arterial line and saline bag.
Barcode scanning of medication packaging may offer an effective safety mechanism for improving picking accuracy, though studies demonstrating this have not been published in critical care. Bar coding will only be functional where the outer packaging is intact, with an up-to-date bar code library linked to all the variety of products used, i.e. unusual medications, ‘specials’ or unlicensed medications may not have recognisable barcodes.
Preparation and Administration
Published evidence indicates that administration errors are more likely to occur with injectable medicines, notably the intravenous route (Keers et al. 2013). Errors are more likely to occur at the preparation stage (Leape and Berwick 2005), in administrations involving multiple steps and especially where there are interruptions or distractions.
Therefore strategies such as the provision of guidance on how to prepare and administer injectable medicines, use of ‘do not disturb’ tabards increasing nurses’ awareness of risk factors involved through training and development programmes and effective second checking processes can be used to minimise these errors.
Smart Pumps Drug Libraries
There is an increasing trend towards better design of systems to limit the human factors that contribute to errors. For medication administration errors, “smart” infusion technology can provide this on a number of levels. Firstly, to enable set, pre-programmed rates of infusions, prescribing needs to be standardised. This reduces the variation in rates and ranges of intravenous medicine prescriptions. The use of dose error reduction software, with the ability to set soft and harm limits can alert to prevent drug calculation errors, manual entry errors when entering dose or volume units or inadvertent pressing of buttons. Introduction can lead to a safe environment for IV administration (HSIB 2019) in ICU where complex infusion and injectable medicines are in high use. Smart infusion pumps have great potential to prevent prescribing as well as administration errors.
A systematic review (Ohashi et al. 2014) reported the benefits of smart pumps are intercepting errors (e.g., wrong rate, dose, or pump settings), reduction of adverse drug events, practice improvements and cost-effectiveness. Problems reported were lower compliance rates, overriding of soft alerts, non-intercepted errors
and the possible use of the wrong drug library.
In practice, unless hard limits are activated, the safety benefits may not be seen (Trbovich et al. 2010). A recent national report highlighted that their introduction can introduce new risks (HSIB 2019). Software is needed to upload the drug library to smart pumps, download data logs (including any errors detected) and monitor the status of each smart pump. Maintaining the required IT infrastructure requires specialist staff roles and often a new skill set.
Ready to Administer Injectables
There are a variety of intravenous (IV) syringe concentrations used throughout the various ICUs, having evolved through custom and practice. With the movement of staff from one unit to another it is desirable to standardise IV infusions, where possible. There is evidence that the manual preparation of syringes on the ICU can vary significantly from what was intended (Dehmel et al. 2011; Adapa et al. 2012). A list of standard syringe concentrations have been published in the UK (ICS and UKCPA CCG 2020). Several manufacturers have launched pre-filled syringes or ‘ready to administer’ vials to correspond with these concentrations, with the intention of reducing the number of manipulations by staff and reducing the likelihood of error. This approach is in accordance with the NPSA alert 20 (NPSA 2007) which stated that, particularly for high risk drugs, hospitals should look for ways to minimise the number of manipulations involved in preparing the product for administration. The drive for standardisation has been helped by the parallel move towards electronic prescribing systems which have templates of standard prescription concentrations and the adoptions of smart pumps with drug libraries (both of which are discussed separately in this article).
However there is a cost implication of adopting these products, which may be offset to an extent by savings in nursing time and reductions in errors. Ready-to-use products require additional space, more attention to ordering and stock rotation to avoid expired stock.
Transition of Care
In a systematic review, Bourne et al. (2022) highlights that the protracted recovery of ICU patients may be further compounded by polypharmacy and care fragmentation. Frequent medication changes, with many chronic medicines discontinued and acute medication commenced, present a patient safety concern, particularly at the point of transitions.
Medicine Reconciliation
The aim of medicines reconciliation in ICU is to ensure that medicines prescribed on ICU admission (if still appropriate) correspond to those that the patient was taking pre- admission. In a previous era, perhaps this was not considered a high priority in the ICU, as the focus was more on the acute aspects of critical illness. It is now recognised that the ICU admission can have a great influence on future drug treatment. Research has showed that medications not prescribed in the ICU, can continue to be omitted on the ward and in some cases on hospital discharge (Eijsbroek et al. 2013). Research indicates that 60-75% of chronic medications are stopped on ICU admission (Campbell et al. 2006) and 80% not restarted on ICU or 30% on hospital discharge (Bell et al. 2006).
Sudden discontinuation of antidepressants such as paroxetine can cause withdrawal phenomena which can contribute to ICU delirium. Omitting to prescribe chronic thyroid replacement therapy in ICU has been associated with negative clinical outcomes (Barrett et al. 2012).
Medication reconciliation on ICU admission is routine in the UK, often carried out by Medicine Management Pharmacy Technicians. Discharge reconciliation at ICU discharge is less widespread, though is equally important. Barriers to this include delayed discharges which are suddenly actioned without an effective review.
Good discharge reconciliation would include documentation for the receiving team any changes to the chronic medication and the ongoing plans for newly introduced medication, for example for insomnia, delirium, atrial fibrillation and corticosteroids.
The evidence currently shows that multicomponent interventions based on staff education and guidelines increase de-prescribing of inappropriate medication at patient hospital discharge by nearly four times (Bourne et al. 2022).Further research is required to establish a process to anchor a quality medication review/communication at ICU discharge.
Discharge Home from the ICU
The ICU can be a less safe zone when unusual practices are undertaken, even though these can be routine on the general wards. Examples of ICU patients who may go home directly from the ICU include some palliative care patients, self-discharges or short-stay post-op recovery patients.
These can be complex discharges where the patient and GP need effective communication to manage detailed thrombosis management plans (which may include arranging anticoagulant follow-up clinics), communication with drug addiction services in the community and a phased reintroduction of chronically used medications. This is outside the comfort zone of many ICU practitioners, but these skills and practices need to be mastered in order to execute these important general ward roles safely.
Monitoring
Guidelines
A suite of local and accessible guidelines can help ICU staff to safely and consistently administer complex and potentially harmful therapy. Easy access to resources such as prescribing guides and local guidelines are likely to reduce prescribing errors. The critique of this approach is that it may detract from individualised medicine (Vincent et al. 2021). But it does at least default practice to a good basic standard, that experts can depart from if the occasion requires.
Miscellaneous
Clinical Pharmacists
The pharmacist’s key role is to promote pharmacotherapy for patients that are safe and effective. Their contribution in critical care has been shown to reduce mortality, length of stay and preventable and non-preventable adverse events (Lee at al. 2019). They influence medication safety across all the stages of medicines use.
The ICU specialist clinical pharmacist (SCP) in the UK are well established members of the multi-disciplinary team. The Core Standards for Intensive Care Units (GPICS 2019) recognises that the ICU pharmacist should have competency in critical care, and the requisite number of SCPs are necessary relative to the size of the unit and the acuity of the patients.
The PROTECTED-ICU UK study report that SCPs made a clinical contribution in 1 in 6 prescriptions on weekdays but 1 in 3 on weekends (Shulman et al. 2015; Rudall et al. 2017). In the 925 patients’ medication reviewed over a 14 day period, 1,393 medication errors were detected. Of these 43% were of moderate impact and 19% were high impact. The types of errors noted in order of prevalence were drugs that were needed but were not prescribed, drugs prescribed that were no longer needed, too high/low doses, error of monitoring and drug interactions/incompatibility. The results showed that 8% of all prescriptions had a medication error which was identified and corrected by the SCP. Of these 19.0% were designated as ‘high’ impact, had they been administered as prescribed and 42.6% were of ‘moderate’ impact. Not surprisingly more experienced SCPs provided clinical contributions that had a higher impact than their junior colleagues. This data provides good evidence that SCP play a vital role in detecting and resolving medication errors.
Learning Environment
Learning from critical incidents is an important element to improve the safety in the ICU. Interdisciplinary review of medication events (Chapuis et al. 2019) can lead to a richer understanding of the contributory factors and to more effective solutions, introduced by those with a good understanding of the issues, with the power and motivation to introduce change. System learning and feedback to staff are also important to provide a safer environment for our patients.
Conclusion
Medication errors are common in the complex environment of the ICU. Each unit will need to embrace a bundle of measures to minimise these errors. The key strategies are discussed in this article. Continuous review of safety is important and also a recognition that an error without a patient consequence should be viewed as an opportunity to learn lessons and implement changes to help minimise the likelihood of more serious events in the future.
Conflict of Interest
None.
References:
Adapa RM et al. (2012) Errors during the preparation of drug infusions: a randomized controlled trial. Br J Anaes. 109(5): 729–734.
Barrett NA et al. (2012) Management of long-term hypothyroidism: a potential marker of quality of medicines reconciliation in the intensive care unit.Int J Pharm Pract. 20(5): 303–306.
Bell CMet al. (2006) Discontinuity of Chronic Medications in patients discharged from the Intensive Care Unit. J Gen Intern Med. 21(9): 937-941.
Bourne RS et al. (2022) Medication-related interventions to improve medication safety and patient outcomes on transition from adult intensive care settings: a systematic review and meta-analysis. BMJ Qual Saf.
Campbell AJ et al. (2006) An observational study of changes to long-term medication after admission to an intensive care unit. Anaesthesia. 61(11):1087–1092.
Chapuis C et al. (2019) Interprofessional safety reporting and review of adverse events and medication errors in critical care.Ther Clin Risk Manag. 15: 549–556.
Cousins D (2007) Safety in doses: medication safety incidents in the NHS : the fourth report from the Patient Safety Observatory. London: National Patient Safety Agency. Available at http://www.nrls.npsa.nhs.uk/resources/?entryid45=61625.
Dehmel C et al. (2011) Do centrally pre-prepared solutions achieve more reliable drug concentrations than solutions prepared on the ward? Intensive Care Med. 37(8): 1311–1316.
Douglass AM et al. (2018) A Randomized Controlled Trial on the Effect of a Double Check on the Detection of Medication Errors. Ann Emerg Med. 71(1): 74-82.
Eijsbroek H et al. (2013) Medication issues experienced by patients and carers after discharge from the intensive care unit. J Crit Care. 28(1): 46–50.
Elliott RA et al. (2021) Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Qual Saf. 30(2): 96–105.
ICS and FICM (2019). Guidelines for the Provision of Intensive Care Services - Edition 2. Available at https://www.ics.ac.uk/ICS/GuidelinesAndStandards/GPICS_2nd_Edition.aspx
Gupta KJ and Cook TM (2013) Accidental hypoglycaemia caused by an arterial flush drug error: a case report and contributory causes analysis. Anaesthesia. 68(11): 1179–1187.
HSIB (2019) Procurement, usability and adoption of ‘smart’ infusion pumps, HSIB. Available athttps://www.hsib.org.uk/investigations-and-reports/procurement-usability-and-adoption-of-smart-infusion-pumps/
ICS and UKCPA CCG (2020) Standard Medication Concentration Guidelines. Available at: https://www.ics.ac.uk/ICU/Guidance/PDFs/Standard_Medication_Concentration_Guidelines
Kane-Gill SL (2018) Advancing Research for Effective Alerts to Avoid Alert Fatigue. Society of Critical Care Medicine (SCCM). Available at: https://sccm.org/Communications/Critical-Connections/Archives/2018/Advancing-Research-for-Effective-Alerts-to-Avoid-A
Keers RN et al. (2013) Causes of Medication Administration Errors in Hospitals: a Systematic Review of Quantitative and Qualitative Evidence. Drug Saf. 36(11):1045–1067.
Latif A et al. (2013) National Study on the Distribution, Causes, and Consequences of Voluntarily Reported Medication Errors Between the ICU and Non-ICU Settings. Crit Care Med. 41(2): 389–398.
Leape LL and Berwick DM (2005) Five years after To Err Is Human: what have we learned? JAMA. 293(19): 2384–2390.
Lee H et al (2019). Impact on Patient Outcomes of Pharmacist Participation in Multidisciplinary Critical Care Teams: A Systematic Review and Meta-Analysis. Crit Care Med. 47(9):1243-1250.
NPSA (2007) Promoting safer use of injectable medicines. Patient Safety Alert 20
https://webarchive.nationalarchives.gov.uk/ukgwa/20180501163752/http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=59812&p=3
Ohashi K et al. (2014) Benefits and risks of using smart pumps to reduce medication error rates: a systematic review. Drug Saf. 37:1011–1020
Rothschild JM et al. (2005) The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 33(8): 1694–1700.
Rudall N et al. (2017) PROTECTED-UK - Clinical pharmacist interventions in the UK critical care unit: exploration of relationship between intervention, service characteristics and experience level. Int J Pharm Pract. 25(4):311–319.
Shulman R et al. (2005) Medication errors: a prospective cohort study of hand-written and computerised physician order entry in the intensive care unit. Crit Care. 9(5): R516-R521.
Shulman R et al. (2015) Pharmacist’s review and outcomes: Treatment-enhancing contributions tallied, evaluated, and documented (PROTECTED-UK). J Crit Care. 30(4): 808–813.
Syed M et al. (2021) Application of Machine Learning in Intensive Care Unit (ICU) Settings Using MIMIC Dataset: Systematic Review. Inform. 8(1): 16.
Trbovich PL et al. (2010) The impact of traditional and smart pump infusion technology on nurse medication administration performance in a simulated inpatient unit. QuaSaf Health Care. 19(5): 430–434.
Valentin A et al. (2009) Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ. 338:b814.
Vincent JL et al. (2021) Equilibrating SSC guidelines with individualized care. Crit Care. 25(1): 397.







