“Martin, 2 years old. Sepsis and pneumoniae. High monitoring systems and modern therapies. A nurse is talking to his parents. A smile and a kind gesture help them in this overwhelming experience. Fear and hope.” This is only an instant picture from a Paediatric Intensive Care Unit (PICU) to illustrate the challenge of critical children care: the fusion of advanced medicine and emotional care.
In the next paragraphs, we will summarise current challenges and opportunities to be addressed in order to improve our practice in the PICU.
Introduction
PICUs have experienced an increase in activity and complexity in the recent decades. Clinical practice has improved dramatically due to new monitoring systems and technological advances in diagnosis and treatment.
Acute medical conditions such as infections, respiratory diseases, injuries, and high complexity surgeries are the most common reasons for admission. Chronic patients often need critical care because of rapid deterioration. Oncological patients frequently require intensive care, and that represents a challenge.
In the era of precision medicine, we highlight the interesting review of Professor Jean Louis Vincent (2019), “treating individuals rather than diseases will necessitate a paradigm change in our approach to diagnosis and management.” This change will not be different in PICU. Not all treatments will be adjusted to all patients. Molecular-based targeting of treatments is currently used in other fields such as oncology and, probably in the future, we will use it to personalise therapy in paediatric critical care.
Mortality in PICU is markedly lower than in adult units, according to figures that vary depending on the country and the allocated resources. Mc Crory et al. (2017) reported a 2.31% mortality rate in the United States and Rashma et al. (2018) reported a 10.58% mortality rate in a PICU in India.
Regarding emotional disturbances, admission into a PICU causes psychological distress for the patients and their families because of the emotional intensity they experience. A family-centred model is essential to provide the best care for children. We will overview the current challenges of managing children in the PICU towards excellence in all fields.
The latest advances on diagnosis and therapy
Moving towards a personalised medicine model is facilitated by recent technology breakthroughs that promote a more accurate management of patients in PICU. Smart PICUs using Big Data predictive analysis including intelligent infusion systems will reduce administration errors (Manrique-Rodriguez et al. 2019), and decision making will be facilitated.
New diagnostic tests or techniques, such as rapid pathogen identification, are decisive in facilitating the choice of the most adequate therapy. Real-time PCR tests to diagnose aetiology and resistance in children with infectious diseases can be a useful tool that can provide additional information for clinical decision making. Current PCR tests are showing promising results in children (Papan et al. 2017; Gowin et al. 2017).
Biomarkers are used as complementary data in the overall assessment of the patient, but in the near future, they could play a key role in defining more precisely the true pathology. In this scenario, biomarkers will be crucial to achieving more targeted therapies according to a molecular-based approach, as Yehya (2019) suggested in an interesting editorial.
Regarding new treatments, novel therapies for oncologic patients have increased the number of “new” patients in our units. As an example, we could mention the case of the chimeric antigen receptor (CAR) T-cell therapy for refractory B-cell acute lymphoblastic leukemia that has led admissions to PICU in order to be treated from the resulting inflammatory response generated (Foster and Maude 2018). These patients are a good example of personalised therapy based on pathophysiology. This therapy has opened a line of treatment for other leukaemia and solid tumours.
There are many new advances being incorporated in the PICU: ECMO, non-invasive ventilation, neutrally-adjusted ventilator assistance, new treatments for recipient of transplants, ventricular assistant devices, neuromonitoring, epilepsy surgery, etc. Future challenges such as the use of 3D impression, the management of emerging infections as Ebola or dengue, multidrug-resistant infections, or immunotherapy will be faced.
All these advances require continuous training of specialised staff, therefore institutions must provide professionals the opportunity for continuous improvement.
Humanisation in the PICU
In our opinion, the field where PICUs have experienced their greatest transformation is in the humanisation of assistance. This cultural change in healthcare mindset is becoming more challenging to professionals than learning and managing new techniques or the latest therapies. In consequence, a major implication and commitment will be required, becoming both a challenge and an opportunity.
The stay in the PICU becomes a stress and anxiety generator for parents. A few years ago, and still now in some cases, parents were allowed to visit their children briefly. Nowadays, most PICUs promote 24-hours access, with clear benefits to children, families, and professionals. In addition, changes in the physical environment of the PICUs have been performed advocating for private rooms instead of the classical open floor units. Our PICU, in Hospital Sant Joan de Déu, Barcelona, has recently shifted from shared rooms to private rooms (Figure 1). This experience has been a challenge with benefits in terms of infection prevention, privacy, decrease of environmental stress and noise. Families can now sleep in the room with their child, hence reducing the fatigue they experience. The main challenge has been the adaptation to a new model where the nurses work in the patient’s box without the previous physical signals and awareness elements indicating the status of other patients and nurses. The concern for patients’ safety in the implementation of this model has been resolved by using a portable alarm system that allows nurses to be permanently aware of patients’ status and easily assist fellow colleagues in case of warning signals.

Programmes focused on improving the hospitalisation experience can be adapted to the PICU. Music therapy, clowns, art or animal therapy have been successfully used in the PICU setting, and it is fair to highlight that these programmes have also had a positive effect on parents’ experience.
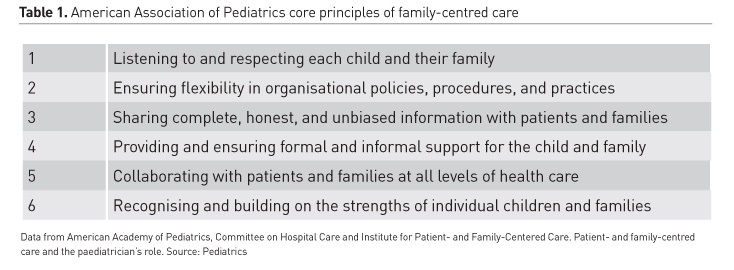
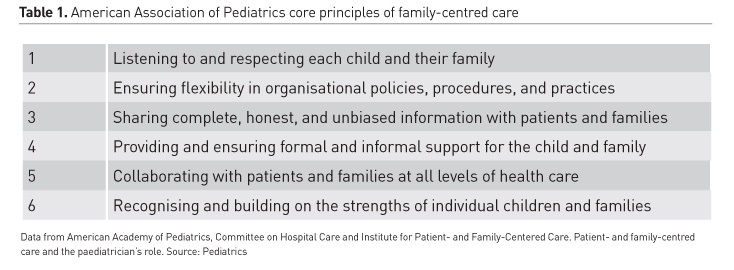
All these changes are included in the family-centred care (FCC) model that promotes the involvement of families in the care of their children. This approach, which has been endorsed by major professional organisations, can deeply influence clinical decisions and patient outcomes (Meert et al. 2013).The American Academy of Pediatrics (AAP) defines FCC as “an innovative approach to the planning, delivery, and evaluation of health care that is grounded in a mutually beneficial partnership among patients, families, and providers that recognises the importance of the family in the patient’s life” (AAP 2012). The PCC is based on six core principles that are listed in Table 1. Currently, FCC is considered the gold standard of care in paediatrics (Ramenzani et al. 2014); however, its implementation can be a challenge when the child is unstable. Nurses play a crucial role in the implementation of FCC. Coats et al. (2018) have recently published the nurses’ reflections on the benefits of FCC in PICU. Nurses must be involved in the decision-making process aiming at a better FCC implementation. The benefits of this model are clear. However some factors and indicators must be taken into account before implementation, especially those concerning stress generation on professionals.
Early mobilisation
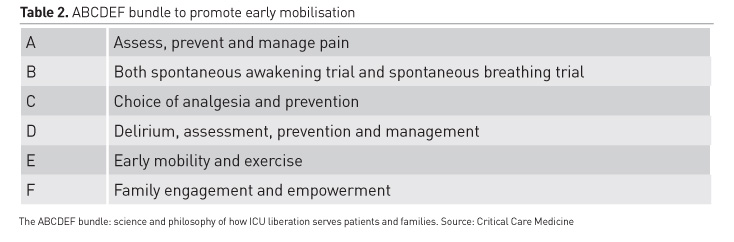
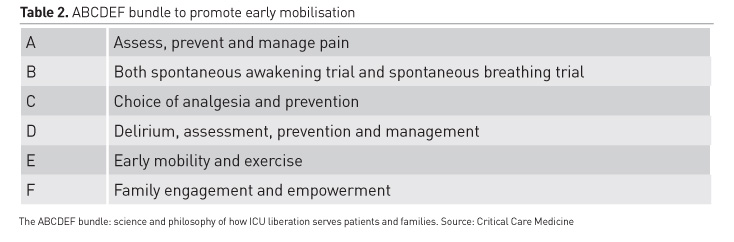
It is well known that survivors of critical care suffer physical and psychological morbidities to deal with. A post-intensive care syndrome can be identified in children including neurocognitive and psychological morbidity (Herrup et al. 2017). Early mobilisation (EM) is one of the actions that can be done to mitigate it. Historically, children in the PICU were profoundly sedated and immobilised. In regards to this issue, there is currently an ongoing transformation promoted by the ICU Liberation. This is a movement that advocates for mobility in terms of allowing critically ill patients to be as safely awake, interactive, and mobile as possible. An ABCDEF bundle is used to achieve this objective (Ely 2017) (Table 2). In adults, it is shown how EM is feasible, safe, improves functional outcomes and increases patient satisfaction (Schweickert et al. 2009; Burtin et al. 2009). Wieckzorek et al. (2016) published their experience with the quality improvement project, PICU Up! This project consists of stratified rehabilitation levels based on the patient’s clinical status ranging from passive range of motion activities to ambulation. PICU Up! is an inspiring project that has encouraged other units to advance in this field. However, we should keep in mind that this project requires a multidisciplinary approach (therapists, physicians, nurses, ancillary staff from child life, and family). The most common barriers to EM in children are the lack of physiotherapy resources, and the concerns about safety. Despite these barriers, EM is beneficial, and each unit has to design their own project according to their resources. In upcoming years we will be faced with required improvements in this area.
Facing death in the PICU: implications for families and professionals
The objective of critical care is to provide support and cure to patients. Despite a low mortality rate in PICU, the manner in which professionals face and deal with this event remains a concern. The death of a child never is experienced as “natural” as it can occur in the adult population, especially in the elderly. Even when death is “expected,” this experience is devastating for parents and stressful for professionals. Initiating palliative care treatment in the PICU confronts specific challenges that require a good understanding between families and health professionals, especially in regards to providing adequate care for a death with dignity. Thus, the need for a multidisciplinary approach and emotional support emerges as a compelling and essential requirement in these cases.
When necessary, religious rites and rituals for parents and family members have to be taken into account in the PICU in order to offer comfort. Communication skills are crucial to help families in this painful moment. Concerning professionals, child care in the PICU can disrupt their psychological balance, and moral distress can also be experienced in circumstances in which the practice is not performed aligned to their sense of duty. Previous structured talks with parents will play an important role in regards to this aspect (Garros et al. 2015). We encourage institutions to provide emotional support to professionals.
Safety in the PICU
Safety in the PICU is a real concern and a major priority for institutions. The diversity of treatments and techniques over the patients make them especially vulnerable to error. In addition, children require a complex pharmacological prescription because of their body weight and this fact adds new possibilities for error.
Actions focused on minimising error and enhancing a climate of safety culture are required. The presence of a clinical pharmacist in the PICU clearly minimises medication errors (Maaskant et al. 2017). Simulation programmes in the PICU are effective both for training and error prevention (Fehr et al. 2017; di Nardo et al. 2018). This strategy should be complemented with mandatory leadership and teamwork specific for safety in the PICU.
Conclusions
Modern PICUs are at the cutting edge in technology and science applied to children’s care. Professionals have to be continuously trained, and it is capital that institutions provide the means and resources for them to update their skills.
Smart PICUs and big data analysis applied to them will be the next frontier to be crossed in terms of challenging patients’ perception on the upcoming personalised medicine model. The newest treatments and the novel support therapies are indicators of the advancement achieved and have also become an encouraging stimuli for us to pursue our mission of paediatric care.
In spite of all the breakthroughs in medicine, some old concerns cannot be dismissed. The well-being of children, families, and professionals must be highlighted as the core of our practice. Transforming a previously hostile environment into a comforting place where to take care of children is one of the most outstanding actions we can offer in the humanisation process of the PICUs. The curative power of a kind word with the best medical assistance, in a context of safety, represents the excellence that all children deserve and society expects.
Abbreviations
AAP American Association of Pediatrics
CART Chimeric Antigen Receptor
ECMO Extracorporeal Membrane Oxygenation
EM Early Mobilisation
FCC Family-centred Care
ICU Intensive Care Unit
PCR Polymerase Chain Reaction
PICU Paediatric Intensive Care Unit
Key points
- Acute medical conditions such as infections, respiratory diseases, injuries, and high complexity surgeries are the most common reasons for admission in the PICU.
- Admission into a PICU causes psychological distress for the patients and their families because of the emotional intensity they experience. A family-centred model is essential to provide the best care for children.
- Smart PICUs using Big Data predictive analysis including intelligent infusion systems will reduce administration errors and facilitate decision making.
- ICU Liberation is a movement that advocates for mobility in terms of allowing critically ill patients to be as safely awake, interactive, and mobile as possible.
- The curative power of a kind word with the best medical assistance, in a context of safety, represents the excellence that all children deserve and society expects.