ICU Management & Practice, Volume 19 - Issue 1, 2019
Overview and focus on regional anaesthesia
Opioid dependency is a serious problem in the ICU. Opioids are effective at providing pain relief because they reduce the perception of the pain signal. At the same time, opioids are associated with respiratory depression, cough suppression, confusion, and drowsiness. In addition, there is a risk of abuse and dependence with opioid drugs.
Despite these risks and associated side-effects, the number of opioid prescriptions continues to increase. Different formulations of opioids are now available, further increasing the risk of abuse and overdose.
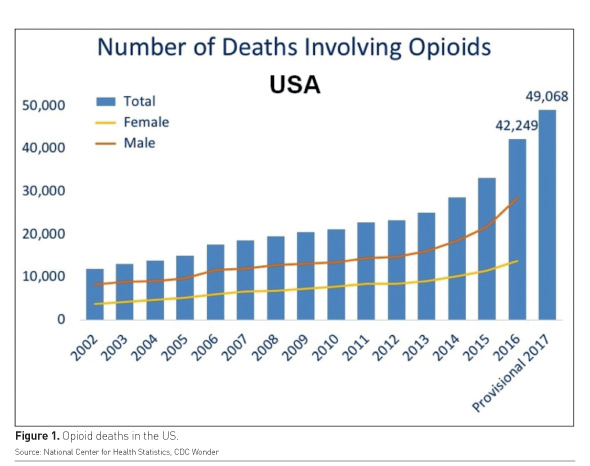
The number of deaths involving opioids is consistently increasing (National Center for Health Statistics). The use of opioids in the ICU and in the post-operative period is very common. Most patients receive opioids even after simple surgeries. Opioid-related deaths are a problem in the U.S. and the opioid epidemic continues to plague the rest of the world as well (Figure 1).
Pain management is not just a strategy to improve patient comfort and patient outcomes, but it is also a means to reduce sedation. However, the type of drugs that are used to manage pain can make a big difference in the level of pain control that is achieved and the quality of patient outcomes that result from the usage of those drugs.
It is important to highlight some key issues that are related to drugs which are used to manage pain. For example, many patients receive opioids (such as morphine, fentanyl, sufentanil, remifentanil) in the post-operative period, even after a simple and classic surgery like total knee arthroplasty. In such patients, the use of a non-opioid drug could be a better option and could protect these patients from opioid-related side-effects.
The practice of analgosedation in the ICU, i.e. using analgesia first instead of sedation is becoming increasingly common. Results of a study published three years ago demonstrated that patients who received more fentanyl and fewer benzodiazepines, and much more dexmedetomidine, but less propofol required lower sedation (Faust et al. 2016). Thus, moving from using total sedation and some analgesics to using more analgesics accompanied by sedatives has proven to be a more effective strategy for reducing sedation. This significant change in the ICU environment is showing results in the form of reduced MV duration and reduced ICU LOS (Faust et al. 2016).
The new paradigm of pain management
It is time to focus on a new paradigm of pain management and to understand the impact of regional anaesthesia and the benefits of multimodal analgesia. Multimodal analgesia refers to a pain management strategy that combines different analgesics with different mechanisms such as opioids, NSAIDs, local anaesthetics, etc. The combined use of these analgesics produces synergistic analgesia and enables clinicians to use lower total doses. This, in turn, reduces the number of side effects. Multimodal analgesia is a more rational approach to pain management and can effectively reduce postoperative pain as well as the use of opioids and sedatives (Jin and Chung 2001).
The new guidelines published in Critical Care Medicine (Devlin et al. 2018) make three primary recommendations for managing pain and balancing sedation:
- Using multimodal analgesia in the ICU. This means that clinicians should use some opiates, and should also use adjunctive therapies such as acetaminophen or nefopam whenever possible. This can help in reducing the number of opioids.
- Using an opiate before the sedatives, and trying to use the lowest effective dose to limit the risk of opioid addiction and dependency in patients.
- Using light sedation in contrast to deep sedation in the critically ill, mechanically ventilated patients.
Findings from a French study (Payen et al. 2013) demonstrated that the use of multimodal analgesia in mechanically ventilated critically ill patients could decrease sedation and delirium and at the same time, avoid the use of opioids and opioid-related side effects (Figure 2). Patients given multimodal analgesia were also more likely to have fewer organ failures and received fewer hypnotics compared to patients who received opioids alone. It is thus evident that the concept of multimodal analgesia must be promoted in the ICU.
Regional anaesthesia: impact on patient outcomes
A study published in JAMA Surgery a few years ago demonstrated that in patients with abdominal aortic aneurysm repair, the overall mortality was different between the group using epidural analgesia and the group using classical analgosedation. Results showed that some of the complications were decreased in the epidural group. The addition of epidural analgesia to general anaesthesia was also associated with long-term survival benefit due to the reduced rates of post-operative complications (Bardia et al. 2016).
Clinical evidence shows that epidural analgesia has some effects on mortality, complications, and morbidity after surgery. The use of epidural analgesia can limit the infusion of opiates and opioid-related complications in ICU patients. The complex and mixed use of sedative agents, associated to analgesia with opiates and the use of regional anaesthesia can help improve patient rehabilitation in the postoperative period. Regional anaesthesia is associated with a composite morbidity score of pneumonia, prolonged ventilator dependency, and postoperative unplanned intubation (Popping et al. 2014).
A study published in Anesthesia and Analgesia (Malekpour et al. 2017) compared no-procedure management, i.e. sedation and opiates versus procedural management with a paravertebral blockade in patients with rib fractures. Results clearly showed differences in mortality and complications. In the patients who received regional analgesia effectively, the rehabilitation was optimised and the use of morphine decreased.
It is thus safe to conclude that the use of multimodal analgesia with non-opioid drugs and regional anaesthesia can have a positive impact on the long-term mortality in patients after big surgeries, as well as optimised pain management and decreased organ dysfunction in these patients.
Key Points
- While opioids are very effective at treating pain, they can also be addictive
- New guidelines make three recommendations for managing pain and balancing sedation: using multimodal analgesia; using an opiate before the sedatives; and using light sedation in contrast to deep sedation in the critically ill, mechanically ventilated patients
- Multimodal analgesia refers to a pain management strategy that combines different analgesics with different mechanisms such as opioids, NSAIDs, and local anaesthetics
- The use of regional anaesthesia can have a positive impact on the long-term mortality as well as optimised pain management in patients after big surgeries
- The addition of epidural analgesia to general anaesthesia was also associated with long-term survival benefit due to the reduced rates of post-operative complications
References:
Bardia A, Sood A, Mahmood F, Orhurhu V, Mueller A, Montealegre-Gallegos M, Shnider MR, Ultee KH, Schermerhorn ML, Matyal R et al. (2016) Combined Epidural-General Anesthesia vs. General Anesthesia Alone for Elective Abdominal Aortic Aneurysm Repair. JAMA Surgery, 151(12):1116-1123.
Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, Pandharipande PP et al. (2018) Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Critical Care Medicine, 46(9):e825-e873.
Faust AC, Rajan P, Sheperd LA, Alvarez CA, McCorstin P, Doebele RL et al. (2016) Impact of an Analgesia-Based Sedation Protocol on Mechanically Ventilated Patients in a Medical Intensive Care Unit. Anesthesia Analgesia, 123(4):903-9
Jakob et al. (2012) Dexmedetomidine vs. midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA, 307(11):1151-60.
Jin F and Chung F (2001) Multimodal Analgesia for Postoperative Pain Control. Journal of Clinical Anesthesia 13:524-539.
Malekpour M, Hashmi A, Dove J, Torres D, Wild J et al. (2017) Analgesic choice in management of rib fractures: paravertebral block or epidural analgesia? Anesthesia and Analgesia, 124:1906-11.
Opioid deaths in the US. National Center for Health Statistics. Available at http://wonder.cdc.gov.
Payen JF, Genty C, Mimoz O, Mantz J, Bosson JL, Chanques G et al. (2013) Prescribing nonopioids in mechanically ventilated critically ill patients. Journal of Critical Care, 28(4):534.e7-12.
Pöpping DM, Elia N, Van Aken HK, Marret E, Schug SA, Kranke P, Wenk M, Tramèr MR et al. (2014) Impact of epidural analgesia on mortality and morbidity after surgery: systematic review and meta-analysis of randomized controlled trials. Annals of Surgery, 259(6):1056-67.
Sun EC, Darnall BD, Baker LC, Mackey S et al. (2016) Incidence of and Risk Factors for Chronic Opioid Use Among Opioid-Naive Patients in the Postoperative Period. JAMA Internal Medicine. 176(9):1286-93.







