ICU Management & Practice, Volume 19 - Issue 1, 2019
How to manage sedation analgesia for patient-centred care in the ICU.
In the concept of patient-centered care, sedation and analgesia have high importance. Intensive care is sometimes invasive and very painful. Patients in the ICU are seriously ill and often suffer from anxiety, agitation, and pain. There is sometimes a need to use deep and prolonged sedation, but that can cause other issues which need to be addressed.
When deep sedation is used, the patient becomes immobile. This can lead to ICU acquired weakness as well as delirium due to the immobilisation of the brain function. Deep and prolonged sedation is associated with worse outcomes, longer duration of mechanical ventilation (MV), longer length of stay (LOS) in the ICU and the hospital, and higher rates of complications such as infections and sometimes even death. It is thus very important to limit the use of deep and prolonged sedation and to understand the use of sedation and pain targets.
Thanks to adequate control of the pain, the level of sedation can be reduced. On the other hand, if the pain is not controlled properly, there is a risk of increased agitation. It is thus very important to use valid and robust tools to assess for agitation such as the Richmond Agitation Sedation Scale (RASS). The RASS score is used to measure the agitation or sedation level and to describe a patient's level of alertness or agitation. It is mostly used in mechanically ventilated patients to avoid over and under-sedation, but it can also be used after in non-intubated patients to assess agitation and delirium as well as side effects of opioids and psychoactive drugs (coma) throughout the ICU stay.
The RASS score is the first step when administering the Confusion Assessment Method in the ICU (CAM-ICU), an effective tool to detect delirium in ICU patients. Clinicians in the ICU should be targeting a RASS score of zero or +1. Anything over +1 can become dangerous for the patient. The RASS target shall be discussed and agreed by the critical care team including nurses and physicians.
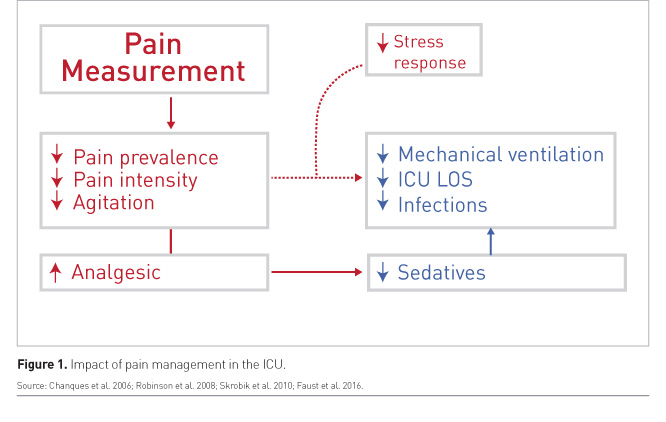
Along with definining and determing sedation targets, it is also important for the critical care team to focus on pain control. Working with a defined target and a continuous assessment of pain leads to more success in decreasing pain prevalence, pain intensity, and agitation. It enables proper and effective use of analgesics. Then sedatives can be reduced leading to a decrease in the duration of mechanical ventilation, ICU LOS, complications, and infections.
Overall, there is significant evidence showing that pain measurement is associated with better outcomes. Better pain management leads to a possible decrease in the stress response. This has been shown by many sequential controlled trials and large multicentre database studies (Figure 1).
Analgosedation
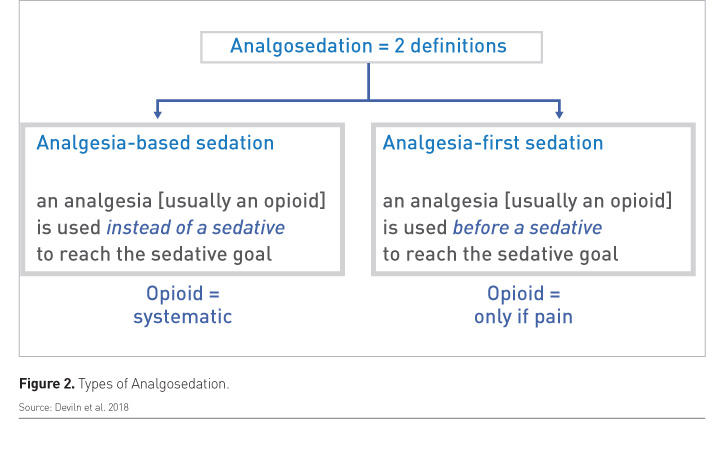
There are two types of analgosedation. One is “analgesia-based sedation” which refers to the use of an analgesic instead of a sedative to reach the sedative goal. The other is “analgesia-first sedation” which refers to the use of an analgesic before a sedative to reach the sedative goal (Figure 2).
There is no defined recommendation on the use of opioids but generally speaking, if there is a patient who is agitated and suffering from pain, an opioid should be used instead of a sedative. By doing so, the need to use sedation will be reduced.
Measuring and managing pain
Different strategies can be used to measure pain depending on the patients. A self-reporting pain scale is generally used in patients who are able to rate their pain using a numeric rating scale (NRS) from 0 (no pain) to 10 (maximum pain) (Chanques et al. 2010). The Behavioural Pain Scales (BPS) and the Critical Pain Observational Tool (CPOT) are used on sedated patients or delirious who are unable to self-report pain scales. These two pain tools are the most validated pain tools in the world.
A study was published a few years ago that compared the use of CPOT and BPS in Critical Care (Chanques et al. 2014). Both of these tools showed the same properties. It is easy to determine whether a non-communicant patient is in pain based on their behaviour.
When the patients suffer from paralysis or are deeply sedated, the most effective way to measure pain is through electrophysiological tools, such as the Analgesia Nociception Index (ANI). This tool analyses heart rate variability. A scale of 0 to 100 is used where 100 is a perfect restful state without pain. When the ANI decreases around the 40s, it is very likely that the patient is in pain.
Pain is experienced by both surgical and medical patients. Studies show that both groups demonstrate pain prevalence and pain intensity during their ICU stay (Kress et al. 2000; Chanques et al. 2017). Surgical patients commonly report pain at the site of the surgery while medical patients often complain of back pain and pain in the limbs. Pain is thus a common occurrence in the ICU and needs to be properly managed so that sedation can be levelled out.
There are some patients in the ICU that still require sedation including those with severe ARDS as well as patients with severe brain injury. However, with proper management, treatment strategies, and the effective use of modern drugs, sedation levels can be minimised in most patients.
Which drugs to use?
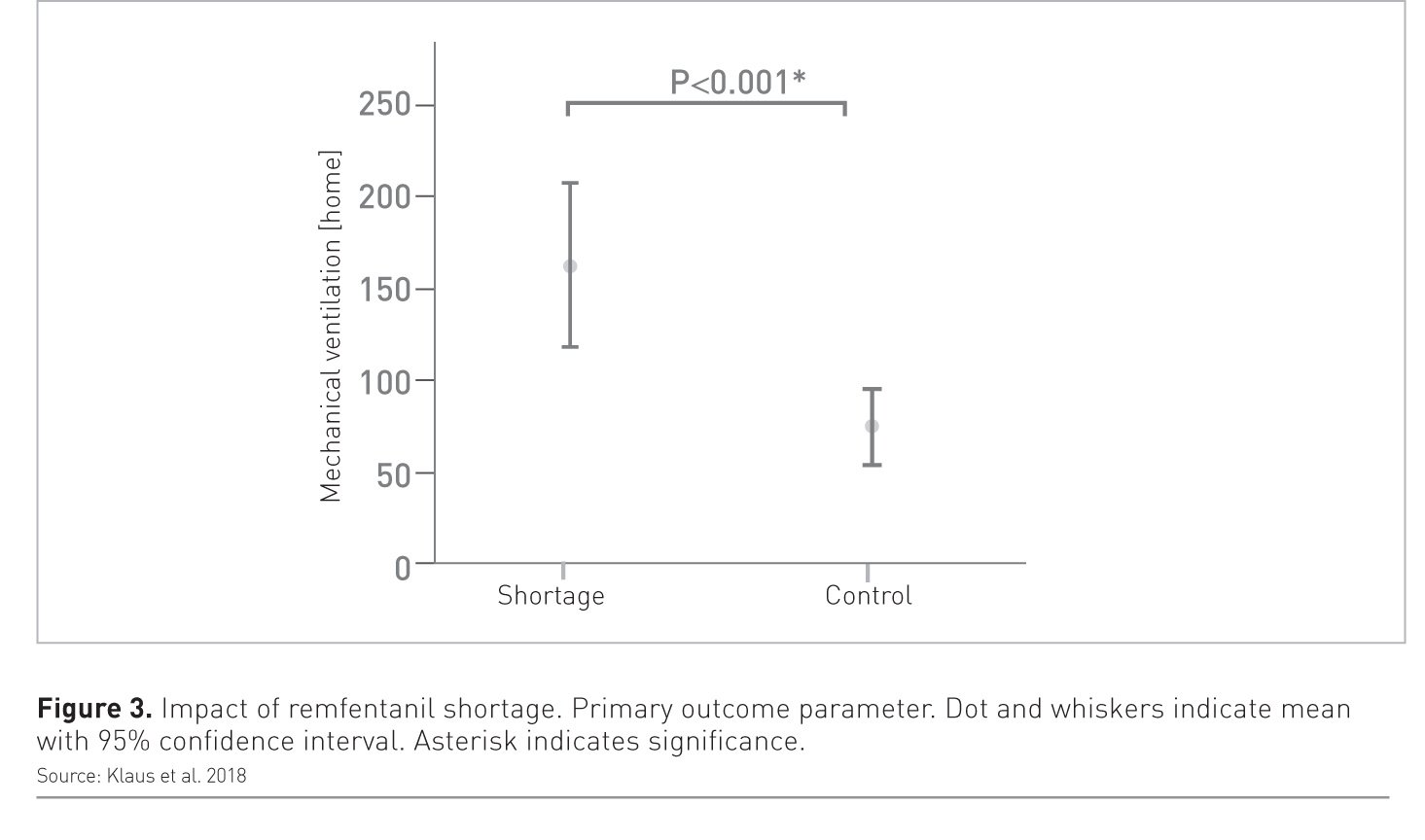
A paper published in Critical Care (Klaus et al. 2018) showed a catastrophic impact of remifentanil supply shortage on mechanical ventilation. Findings showed a very high duration of MV in patients who experienced the period of remifentanil shortage and were forced to use another drug instead (Figure 3). This indicates the impact that the chosen drug can have on a patient’s condition and outcome.
Guidelines recommend that benzodiazepines should probably be avoided for sedation. Propofol and dexmedetomidine should be given preference. For analgesics, morphine should be avoided whenever possible as there is a risk of overdosing in patients with acute renal failure. The use of multimodal analgesia should probably be promoted so that opioids are not overused and the overall pain management effort is more effective (Devlin et al. 2018).
Using the bundled approach (ABCDEF)
The ABCDEF bundled approach to pain management is an evidence-based guide for clinicians in the ICU to enable them to optimise patient recovery and outcomes (Pandharipande et al. 2010). The ABCDEF bundle includes:
Both Spontaneous Awakening Trials (SAT) and Spontaneous Breathing Trials (SBT);
Choice of analgesia and sedation drugs;
Delirium: Assess, prevent, and manage;
Early mobility and exercise;
Family engagement and empowerment.
Some of the key benefits of the ABCDEF bundle include:
- Empowerment of clinicians and families
- Well-rounded patient care
- Optimal resource utilisation
- Better pain control
- Improved physical recovery
- Improved mental health
The concept of eCASH
The eCASH concept is based on the premise of delivering patient-centred care without excessive sedation. The strategy can be regarded as an evolution of the Pain, Agitation and Delirium guidelines, hence the mnemonic eCASH – Early Comfort using Analgesia with a minimum of Sedatives and a maximum of Humanity. Providing effective pain relief to patients in the ICU is the first priority when implementing eCASH. This pain relief can be achieved through the use of multimodal analgesia. Sedation should be secondary to pain relief and whenever possible, should be based on drugs that can be titrated to prespecified sedation targets (Vincent et al. 2016).
Key Points
- Deep sedation can lead to ICU acquired weakness as well as delirium due to the immobilisation of the brain function
- Prolonged sedation is also associated with worse outcomes, longer duration of mechanical ventilation (MV), longer length of stay (LOS) and higher rates of complications
- The use of analgosedation can help manage pain as well as reduce the need for sedation
- Fixing sedation targets and measuring pain is important for more effective patient management
- The Richmond Agitation Sedation Scale (RASS) is used to measure the agitation or sedation level and to describe a patient's level of alertness or agitation
- The ABCDEF bundled approach is the key to effective pain management and improved patient outcomes
References:
Chanques G, Jaber S, Barbotte E, Violet S, Sebbane M, Perrigault PF, Mann C, Lefrant JY, Eledjam JJ et al. (2006) Impact of systematic evaluation of pain and agitation in an intensive care unit. Critical Care Medicine, 34(6):1691-9
Chanques G, Viel E, Constantin JM, Jung B, de Lattre S, Carr J, Cissé M, Lefrant JY, Jaber S et al. (2010) The measurement of pain in intensive care unit: comparison of 5 self-report intensity scales. Pain, 151(3):711-21.
Chanques G, Pohlman A, Kress JP, Molinari N, de Jong A, Jaber S, Hall JB et al. (2014) Psychometric comparison of three behavioural scales for the assessment of pain in critically ill patients unable to self-report. Critical Care, 18(5):R160.
Chanques G, Conseil M, Roger C, Constantin JM, Prades A et al. (2017) Immediate interruption of sedation compared with usual sedation care in critically ill postoperative patients (SOS-Ventilation): a randomised, parallel-group clinical trial. The Lancet. 5(10):795-805.
Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, Pandharipande PP et al. (2018) Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation,
Faust AC, Rajan P, Sheperd LA, Alvarez CA, McCorstin P, Doebele RL et al. (2016) Impact of an Analgesia-Based Sedation Protocol on Mechanically Ventilated Patients in a Medical Intensive Care Unit. Anesthesia Analgesia, 123(4):903-9
Klaus DA, de Bettignies AM, Seemann R, Krenn CG, Roth GA et al. (2018) Impact of a remifentanil supply shortage on mechanical ventilation in a tertiary care hospital: a retrospective comparison. Critical Care, 22:267.
Kress et a Kress JP, Pohlman AS, O'Connor MF, Hall JB et al. (2000) Daily Interruption of Sedative Infusions in Critically Ill Patients Undergoing Mechanical Ventilation. New England Journal of Medicine, 342:1471-1477.
Pandharipande P, Banerjee A, McGrane S, Ely EW et al. (2010) Liberation and animation for ventilated ICU patients: the ABCDE bundle for the back-end of critical care. Critical Care, 14(3):157.
Payen JF, Genty C, Mimoz O, Mantz J, Bosson JL, Chanques G et al. (2013) Prescribing nonopioids in mechanically ventilated critically ill patients. Journal of Critical Care, 28(4):534.e7-12.
Robinson BR, Mueller EW, Henson K, Branson RD, Barsoum S et al. (2008) An analgesia-delirium-sedation protocol for critically ill trauma patients reduces ventilator days and hospital length of stay. Journal of Trauma, 65(3):517-26.
Skrobik Y, Ahern S, Leblanc M, Marquis F, Awissi DK et al. (2012) Protocolized intensive care unit management of analgesia, sedation, and delirium improves analgesia and subsyndromal delirium rates. Anesthesia Analgesia, 111(2):451-63.
Vincent JL, Shehabi Y, Walsh TS, Pandharipande PP, Ball JA et al. (2016) Comfort and patient-centred care without excessive sedation: the eCASH concept. Intensive Care Medicine, 42(6):962-71.







