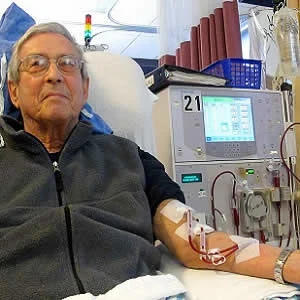
It is estimated that 22–57% of critically ill patients develop acute kidney injury (AKI) during their hospitalisation. The increasing incidence of AKI has the immediate effect of a growing need for renal replacement therapy (RRT). However, evidence on how to manage RRT in critically ill patients with AKI remains limited because of ambiguous study results and low standardisation, says a review paper in the journal Current Opinion in Anesthesiology.
RRT is still "the gold standard" for treating patients suffering from severe AKI, and beyond, it is the only reliable therapeutic option, according to the paper published by Melanie Meersch, MD and Alexander Zarbock, MD, both from the Department of Anaesthesiology, Intensive Care and Pain Medicine, University of Munster, Munster, Germany.
Critically ill patients are exposed to multiple factors known to deteriorate kidney function. Especially severe fluid overload is strongly associated with worse outcome and may be considered as a trigger for initiating RRT. Apart from its detoxification function, the primary goals of RRT are the achievement and maintenance of electrolyte, acid–base, and fluid balance.
The best management of RRT, as the paper notes, is still a subject of controversy. Since the publication of the "kidney disease: improving global outcomes" (KDIGO) guidelines for AKI in 2012, many research efforts have been undertaken, but the results are contradictory and unclear. "Ongoing trials regarding optimal timing and anticoagulation of RRT will hopefully bring new insights to improve the practice of RRT," the authors say.
They explain that in the face of life-threatening complications, the decision of when to initiate RRT is self-evident. In the absence of such complications, severe fluid overload is a reasonable trigger for the initiation of RRT. In certain circumstances, early initiation of RRT is superior to a more delayed start, the authors point out.
"By providing better haemodynamic stability and superior control of fluid balance continuous RRT is the first choice therapeutic tool as compared with intermittent techniques. The femoral and jugular veins are the preferred insertion sites for temporary catheters. Although data are still weak, there is some preliminary evidence that regional citrate anticoagulation is superior to systemic heparinisation," Drs. Meersch and Zarbock write.
In some countries, however, practitioners do not use any anticoagulation for continuous RRT at all, although it has been shown that anticoagulation prolongs filter life time, the authors add.
Source: Current Opinion in Anesthesiology
Image Credit: Anna Frodesiak
References:
Melanie, Meersch et al. (2018) Renal replacement therapy in critically ill patients: who, when, why, and how. Current opinion in Anesthesiology. doi: 10.1097/ACO.0000000000000564
Latest Articles
AKI, hospitalisation, Renal replacement therapy, critically ill patients
It is estimated that 22–57% of critically ill patients develop AKI during their hospitalisation. The increasing incidence of AKI has the immediate effect of a growing need for renal replacement therapy (RRT). However, evidence on how to manage RRT in crit