ICU Management & Practice, Volume 17 - Issue 2, 2017
According to the World Bank classification, Tunisia is considered a lower middle-income country, corresponding to a country with a Gross National Income (GNI) per capita between USD1,026 and USD4,035 (World Bank 2015). The economic growth of Tunisia has been slowed following the 2011 Arab Spring, which was initiated in this country. Despite economic and political constraints, which have been exacerbated by the Arab Spring, Tunisia continues to capitalise on the choices made upon its independence in 1956, focusing on human development. Education and health for all was the leitmotif in that period, with free and compulsory public schooling, and free access to healthcare in its preventive and curative dimensions. As a result, the country still ranks among the first emerging countries in terms of the human development index (wealth), a composite of four components: life expectancy at birth, expected years of schooling, mean years of schooling, and GNI per capita. In 2016 Tunisia ranked 97 within the strata of countries with high human development (United Nations Development Programme 2016). As to healthrelated indicators, Tunisia performs among the best countries within its category, in terms of life expectancy (which rose from 70.3 years in 1990 to 75.6 in 2013), maternal mortality, fertility (which dropped from 5.2 children per woman in 1981 to 2.3 children by 2013), infant mortality etc. (GBD 2015 Child Mortality Collaborators 2016; GBD 2015 Maternal Mortality Collaborators 2016; GBD 2015 Risk Factors Collaborators 2016; GBD 2015 SDG Collaborators 2016; GBD 2015 Disease and Injury Incidence and Prevalence Collaborators 2016). Tunisia faces a striking epidemiological change with an important decline in communicable diseases and an increase in non-communicable diseases, including diabetes (one in six Tunisians suffers from diabetes in 2015), overweight (involving 60% of citizens over 35 years), vascular diseases, and cancer.
Intensivists and Intensive Care Societies
Four schools of medicine, distributed from the capital Tunis to the south, are in charge of the training of more than 1500 students each year, of whom almost one quarter specialise after MD graduation. Regarding intensive care medicine practice in Tunisia, there are two pathways of specialisation, which were started only by the early 1980s: anaesthesiology and surgical intensive care medicine, and medical intensive care medicine, with a curriculum of 5 years for the former and 4 years for the latter. This makes intensive care medicine the sole medical specialty with two parallel curricula, a scheme that is similar to that existing in France, although medical intensive care medicine has been a supra-specialty in France thus far. As a consequence, two societies of intensive care medicine exist in Tunisia: STAAR (Société Tunisienne d’Anesthésie Analgésie & Réanimation) for the first curriculum, and ATR (Association Tunisienne de Réanimation) for the medical intensivists. These societies have long ignored each other, and organise their own congresses, although a recent rapprochement has been made with the organisation of a common scientific day. Yet intensivists on both sides have common interests and challenges they could have addressed in a united way with the health authorities. Among the common problems are the lack of legislation defining intensive care medicine, the need for ICU beds, architectural standards, the minimal and maximal capacity of ICUs, the standards in terms of biomedical equipment, workforce, and operating procedures. Another area that could have brought the intensivists together is the lack of reimbursement for intensive care in the private sector, which imposes a monstrous out-of-pocket financial burden on citizens who choose this sector, and the undervaluation of reimbursement of an ICU admission in the public sector.
ICU Bed Capacity and Distribution
Tunisia’s healthcare system includes three levels of care: primary, with a network of more than 2000 basic health centres; secondary, with 109 district hospitals; and tertiary, with 33 regional hospitals and 24 modern teaching hospitals (Centre Hospitalo-Universitaire) (République Tunisienne Ministère de la Santé 2016). Tunisia’s private healthcare sector acccounts for no less than 49% of doctors in the country (split into more than 3100 general physicians, and more than 3600 specialised physicians), and more than 90 private clinics, with 75 new clinics expected to be built by 2025 (Oxford Business Group 2016). The public sector remains the primary healthcare provider in Tunisia with 31,936 beds, accounting for 87% of hospital bed capacity. The Tunisian health system counts around 500 ICU beds distributed between the public sector (240 beds corresponding to a ratio of 7.5/1000 acute care beds) and the private sector (around 280 beds corresponding to a ratio of 58/1000 acute care beds). Compared with global trends worldwide, this ratio for public/private ICU beds seems anachronistic, since the global trend is characterised by the gradual reduction in so-called “cold” beds with the increase in ICU beds, a figure that the private sector seems to have understood both in the distribution of its beds offer, and in its functioning, aiming at minimising the frequency and duration of hospitalisation.
These beds are organised in ICUs of variable size and organisation. In the private sector ICU beds are usually assembled in open ICUs of small (4 beds) to medium-sized units (12 beds). These ICUs are usually managed by anaesthesiologists recruited on a full-time basis by the clinics, cumulating both the operative activity of anaesthesia within the operating room, and the management of cases (more or less rare) of patients requiring intensive care whether or not in relation to surgery. Anaesthesiologists working in the private sector have a close relationship with specialists from a variety of backgrounds, and perform all patient conditioning procedures (catheterisation, drainage etc.), together with the management of all aspects of artificial ventilation.
Things are quite different in the public sector and resemble more the European reality. In the teaching hospitals, the ICUs are usually bigger than in the private sector (at least 8 beds), and are staffed by substantially more intensivists. ICUs are more often specialised either in the surgical field (and managed by anaesthesiologists in this case), or in the medical field (and managed by medical intensivists therefore). In the largest university hospitals in the country (5-6 hospitals plus the principal military hospital in Tunis), these two types of ICUs usually coexist, in addition to the coronary care unit. In this case, surgical ICUs take care of all patients requiring intensive care in the perioperative period, in addition to trauma patients, whereas non-operative patients are admitted to the medical ICU. In smaller academic hospitals, as well as in non-university regional hospitals, only one type of ICU exists, which theoretically assures any kind of intensive care.
Quality of Care
The quality of patient care achieved in Tunisian ICUs can be inferred from two interesting studies. In a study aiming at the validation of severity scores in use in ICUs, Nouira et al. compared the performance of the scores Simplified Acute Physiology Score (SAPS II), Acute Physiology and Chronic Health Evaluation (APACHE II), Mortality Prediction Model (MPM0) and MPM24 in a Tunisian population of patients admitted to three ICUs (Nouira et al. 1998a). All models showed an acceptable discrimination power, but were inadequately calibrated. All models tended to underestimate actual mortality (high standardised mortality ratios [SMRs]). Beside an actual difference in the quality of care between Tunisian and western ICUs, some other factors might have accounted for the discrepancy between predicted and observed mortality rates. These might be putative differences in the disease leading to ICU admission (case mix), lead time bias, or availability of resources. Indeed, the main observed difference was the higher proportion of medical admissions in the Tunisian dataset (84.2%) in comparison to European and North American reports, a fact that might have contributed to an under-prediction of death, as it is acknowledged that surgical patients have actually lower mortality risks than medical patients.
See Also: Informatics Drives Radiology Today – Interview with Hassen Gharbi
An interesting benchmarking study compared variations in intensive care utilisation and outcome in relation to variations of costs in two large university hospitals (Monastir in Tunisia, and Créteil in France) (Nouira et al. 1998b). The working hypothesis was that since the Tunisian ICU medical staff had received post-doctoral training in that French unit and should have similar skills, any difference in the therapeutic approach should be due mainly to resource limitations as both countries had striking differences in GNI and the share of GNI spent in healthcare. This study showed that Tunisian patients received less treatment during a shorter length of stay, leading to overall lower costs than French patients but with higher ICU mortality. Regarding cost-effectiveness profiles, it was similar in the low range severity group, but it was significantly poorer in Tunisia regarding the middle range of severity. However, in the highest severity range, there was a trend toward increased mortality and SMR in the Tunisian ICU, which could be viewed as more efficient from an economical standpoint. The study also showed an overall younger age and better prior health status of Tunisian ICU patients, reflecting a Tunisian policy of actively restricting ICU admission where the ICU bed shortage put a greater triage pressure on Tunisian physicians. The situation has probably changed nowadays with a high number of new ICU beds operated, at least in the private sector, making such benchmarking studies welcome.
Research and Research Networks
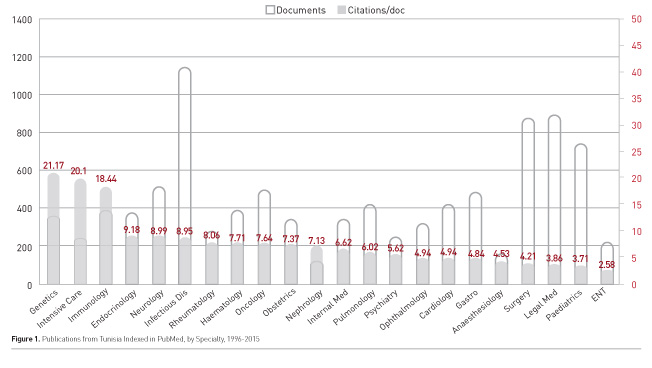
Despite its young age relative to well-established specialties, Tunisian intensive care medicine is one of the local disciplines with a strong tradition of research and publication. This research concerns both diseases with a high local prevalence/ specificity (scorpionism, toxicology, traumatology), but also diseases that concern the whole community of intensivists throughout the world. Figure 1 shows the distribution among major specialties of publications indexed in PubMed, both as an absolute production (white bars) over the period (1996-2015), and the average citation per paper (grey). Intensive care medicine has one of the best quality of publication with one of the highest ratios of citations/paper. In spite of some sporadic attempts, there is no Tunisian research network in the intensive care field. We should admit that the culture of networking is almost non-existent in Tunisian medical research. This culture is indeed somewhat new worldwide, but nothing is done from the institutional side to federate skills in a specific field, or around a promising research project. There are neither financial incentives nor obligations favouring such groupings to be made.
Nevertheless, many Tunisian teams have been involved in international networking, particularly on mechanical ventilation, with several international publications involving Tunisian teams (Esteban et al. 2008; Ferguson et al. 2005; Nin et al. 2017; Delclaux et al. 2000; Maggiore et al. 2010; Jolliet et al. 2017).
Challenges and Opportunities
Like many emerging countries throughout the world Tunisia faces the challenge of brain drain in the field of medicine and particularly in that of critical care medicine. At the end of their specialisation curriculum, Tunisian residents, especially those belonging to intensive care medicine, usually validate 1 to 2 years of their curriculum in a European country (usually France). While this mobility used to be informal, occurring through an arrangement between supervisors in both countries, it is now integrated within the framework of the French diploma of specialisation (DFMS), in which Tunisian (and more generally North African) residents pass a formal examination in the French Embassy and then are assigned to functional posts managed by the University of Strasbourg as required by local needs in the specialty workforce. This new system is considered a major regression when compared to the previous mode of exchange which, even if it was less well organised, was nevertheless satisfactory for the desire for training of the residents who were able to join medical teams in highly trained services in France, whereas with the new system, they find themselves more often in places lacking supervision where they provide services that are shunned by French physicians.
The brain drain continues even after the residency period with a strong attraction put on the young medical specialists of the country to join the French system through an equivalence contest where the performance of the Tunisian doctors is unanimously recognised. This brain drain is present in all disciplines, but is particularly high in high-stress specialties such as anaesthesiology and critical care medicine.
Another challenge intensive care medicine has to face in the next years is the unification of the curriculum leading to intensive care specialty. It seems illogical that residents come to the exercise of intensive care through two separate curriculums, that of anaesthesiology and surgical ICM, and the medical ICM curriculum. A unified way should be identified in order to have one single and efficient curriculum.
Conflict of Interest
Lamia Ouanes-Besbes declares that she has no conflict of interest. Mustapha Ferjani declares that he has no conflict of interest. Fekri Abroug declares that he has no conflict of interest.
References:
Delclaux C, L’Her E, Alberti C et al. (2000) Treatment of acute hypoxemic nonhypercapnic respiratory insufficiency with continuous positive airway pressure delivered by a face mask: A randomized controlled trial. JAMA, 284(18): 2352-60.
Esteban A, Ferguson ND, Meade MO et al. (2008) Evolution of mechanical ventilation in response to clinical research. Am J Respir Crit Care Med, 177(2): 170-7.
Ferguson ND, Frutos-Vivar F, Esteban A et al. (2005) Airway pressures, tidal volumes, and mortality in patients with acute respiratory distress syndrome. Crit Care Med, 33(1): 21-30.
GBD 2015 Child Mortality Collaborators (2016) Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet, 388(10053): 1725-74.
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators (2016) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545-602.
GBD 2015 Maternal Mortality Collaborators (2016) Global, regional, and national levels of maternal mortality, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet, 388(10053): 1775-812.
GBD 2015 Risk Factors Collaborators (2016) Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet, 388(10053): 1659-724.
GBD 2015 SDG Collaborators (2016) Measuring the health-related Sustainable Development Goals in 188 countries: a baseline analysis from the Global Burden of Disease Study 2015. Lancet, 388(10053): 1813-50.
Jolliet P, Ouanes-Besbes L, Abroug F et al. (2017) A multicenter randomized trial assessing the efficacy of helium/oxygen in severe exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med, 195(7): 871-80.
Maggiore SM, Richard JC, Abroug F et al. (2010) A multicenter, randomized trial of noninvasive ventilation with helium-oxygen mixture in exacerbations of chronic obstructive lung disease. Crit Care Med, 38(1): 145-51.
Nin N, Muriel A, Penuelas O et al. (2017) Severe hypercapnia and outcome of mechanically ventilated patients with moderate or severe acute respiratory distress syndrome. Intensive Care Med, 43(2): 200-8.
Nouira S, Belghith M, Elatrous S et al. (1998a) Predictive value of severity scoring systems: comparison of four models in Tunisian adult intensive care units. Crit Care Med, 26(5): 852-9.
Nouira S, Roupie E, El Atrouss S, Durand- Zaleski I, Brun-Buisson C, Lemaire F, et al. (1998b) Intensive care use in a developing country: a comparison between a Tunisian and a French unit. Intensive Care Med, 24(11): 1144-51.
Oxford Business Group (2016) Tunisian health sector to undergo overhaul. In: The report: Tunisia 2016. [Accessed: 16 May 2017] Available from oxfordbusinessgroup.com/overview/ annual-check-solid-foundation-sector-readyoverhaul République Tunisienne Ministère de la Santé (2016) Structures publiques de santé en tunisie. [Accessed: 16 May 2017] Available from santetunisie. rns.tn/fr/carte-sanitaire/structurespubliques- de-sante-en-tunisie
United Nations Development Programme (2016) Human Development Report: Tunisia. [Accessed: 16 May 2017] Available from http:// hdr.undp.org/en/countries/profiles/TUN World Bank (2015) World development indicators: Tunisia. Group Country Survey 2015 2015 [Accessed: 16 May 2017] Available from data. worldbank.org/country/Tunisia









