ICU Management & Practice, Volume 23 - Issue 3, 2023
Reducing the carbon footprint in healthcare is a requirement for guaranteeing the best future for humanity. Here we suggest that the carbon footprint be assessed as a potential endpoint for future trials in critical care.
Environmental Impact in Critical Care
The climate crisis is a threat to global health. The temperature of the atmosphere has been rising exponentially since the industrial revolution due to anthropogenic greenhouse gas emissions. The Intergovernmental Panel on Climate Change special report estimates that a drastic reduction in these emissions is required to limit global warming and its consequences on human health. The Paris Agreement, which was signed in 2015 proposed to limit warming in 2050 to +1.5°C compared to the pre-industrial era.
While the Hippocratic oath to “first do no harm” guides physician practice, the healthcare system is a major contributor to climate change (Lenzen et al. 2020). In industrialised countries, it is responsible for 3 to 10% of national greenhouse gas emissions. The carbon footprint of health systems should be calculated in each country in order to implement targeted measures to reduce it (Booth 2022). An Australian study performed from 2014 to 2015 highlighted that the carbon footprint attributed to healthcare in Australia was 7% (Malik et al. 2022). This covers a broad range of activities such as building supplies, patient travel, staff commute, medicines and chemicals, medical devices, non-medical equipment, and other supply chain actions. NHS England estimated that pharmaceuticals and medical devices represented around 20% and 10% of the total carbon footprint of their healthcare system (NHS England 2020).
The reference unit used to account for greenhouse gas emissions is the carbon dioxide (CO2) equivalent (CO2-e). This corresponds to the warming power of each greenhouse gas relative to CO2, which is the reference gas. In the hospital, efforts are required in all sectors. In the operating room, halogenated gases are strong producers of greenhouse gas emissions. Chambrin et al. showed that the setup of sustainable anaesthesia groups, providing information meetings about the carbon footprint of inhaled halogenated anaesthetics, was associated with a significant decrease in the carbon footprint related to halogenated anaesthetics (Chambrin et al. 2023). In the field of pulmonary diseases, the change in pressurised metered dose inhalers provided better treatment and outcomes while reducing greenhouse gas emissions (Pernigotti et al. 2021).
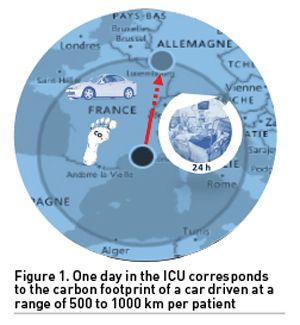
Intensive care units (ICUs) are important consumers of material and energy resources. Their greenhouse gas emissions are thus particularly high, representing, in an observational study conducted in a U.S. hospital, 1% of the hospital total by relative staffing intensity (Prasad et al. 2022). In a study of patients in septic shock, McGain et al. (2018) calculated the average daily greenhouse gas emissions in ICUs at Barnes Jewish Hospital, St. Louis, MO, U.S. and Footscray Hospital, Melbourne, Vic, Australia (McGain et al. 2018). They found that the daily greenhouse gas emissions were 178 kg CO2-e and 88 kg CO2-e in the U.S. and Australian ICUs, respectively. They concluded that the carbon footprints of the ICUs were mainly dependent on the energy used for heating, ventilation and air conditioning. Another estimate of the carbon footprint in a U.S. hospital showed 138 kg CO2-e per bed day for ICU patients (Prasad et al. 2022). This corresponds to the emissions of a car driven 500 to 1000 km per patient per day (Figure 1). This made consumables, which have been regarded in non-ICU studies, relatively less important in this setting.
Beyond CO2, other environmental factors should be considered: air, soil and water pollution, ecotoxicity of drugs, and excessive water consumption. In an ICU of a U.S. hospital, it was calculated that 300L of water usage and 4 m2 of agricultural land occupation were used per patient and per day (Hunfeld et al. 2023). Five practices were clearly identified as having a strong impact on the environment: non-sterile gloves, isolation gowns, bed liners, surgical masks and syringes. Regarding those multiple categories of pollution, decision-makers have to rank their importance and choose their poison. As climate change is an existential risk to each of us, it has been ranked as the impact category of greatest concern in a long-term perspective. At a time of climate crisis, we consider that this impact should no longer be ignored when evaluating our practices (Muret et al. 2019). The scientific literature should include it as an outcome in its own right.
Towards a New Meaningful Outcome in Clinical Research
Clinical research needs to assess procedures, treatments, and strategies based on defined outcomes. For critically ill patients, mortality – in-ICU, in-hospital, at day-28, at day-90 – is the most often measured outcome. In a recent study, ICU mortality was approximately 20%, with an additional mortality rate of 17% in the year after ICU discharge, making this outcome really accurate (Atramont et al. 2019). However, other outcomes can also be relevant. Indeed, quality of life may be impaired after surviving a critical illness; hence, quality of life should be considered among potential outcomes in ICU patients (Herridge and Azoulay 2023). To integrate this aspect in the analysis of outcomes, days at home could be considered an important patient-centred outcome in future critical care trials (Martin et al. 2023). For specific treatments, procedures or strategies, the measure of costs of the ICU stay, under the labelling pharmaco-economic studies, served as an outcome (Oude Lansink-Hartgring et al. 2023). The choice between two strategies that are similar in terms of clinical outcomes may be driven by a reduction in costs associated with one of these strategies.
In our view, the carbon footprint of an ICU stay - actually, the carbon footprint of each treatment or procedure during an ICU stay - should be considered as a potential outcome in future critical care trials to affect the medical decision. A think tank - the Shift Project - suggested that the purchase of pharmaceuticals and medical devices should be based on the least environmental impact for a similar level of quality of care. This would make it possible to choose the same quality of care and the most efficient strategy in terms of the environment.
In medical ethics, two different approaches help guide medical decisions. In the deontological approach, individual dignity is at the heart of the process. Everything must be done to respect it. In the utilitarian approach, the aim should be the well-being of the largest number of individuals, even if it means limiting the care of a single individual. This is usually the approach preferred in a health crisis, such as the COVID-19 crisis. In fact, we are crossing a climate crisis, which is confirmed by a series of evidence. Applying the utilitarian approach to this crisis should lead us to think about the excessive environmental impact of strategies which do not systematically affect patient outcomes
.
Barratt and McGain (2021) elegantly put into question the impact of overdiagnosis - detection of harmless conditions that could be safely left underdiagnosed and untreated - on the environment, suggesting that climate change requires efforts to improve the relevance of care. In a comparative non-randomised clinical trial, the use of a portable ultrasound device increased the rate of immediate adequate diagnosis from 80% to 94%. In parallel, there was a decrease in supplemental examinations and the number of interventions, probably reducing the carbon footprint for each patient associated with improved outcomes (Zieleskiewicz et al. 2021). The balance between the benefit and risks of each decision should be assessed on an environmental scale. Obviously, it is unthinkable at this time to reduce the quality of care to reduce our environmental impact. Nevertheless, we believe that, for the same quality of care, the least polluting strategy should always be preferred in the management of intensive care patients.
In the long term, this approach also has a positive impact on public health. Indeed, recent data show that there are health co-benefits to implementing environmental policies. These data show that the implementation of environmental policies is accompanied by co-benefits on the health of the population (Milner et al. 2023). For example, some modelling-studies have shown that reducing the use of coal for electricity generation will result in health benefits that exceed the economic cost of decarbonisation policies through reduced local air pollution.
Whereas its goal is to ameliorate the global health of populations, healthcare systems participate in increasing GHG emissions, which have, in turn, detrimental effects on the health of populations. Our generations have to break this vicious circle by reducing these emissions without deteriorating the level of care. This dual accountability invites reassessing the procedures in critical care under the light of GHG emission reduction. This implies not only choosing the less consuming procedures but also improving the diagnosis accuracy and avoiding overdiagnosis, leading to no unnecessary investigations and treatments. Finally, we propose to include the carbon footprint as a pharmaco-ecological outcome for future clinical trials to determine the best strategies both at the patient and collective levels.
Conflict of Interest
None.
References:
Atramont A, Lindecker-Cournil V, Rudant J et al. (2019) Association of Age With Short-term and Long-term Mortality Among Patients Discharged From Intensive Care Units in France. JAMA Netw Open. 2(5):e193215.
Barratt A, McGain F (2021) Overdiagnosis is increasing the carbon footprint of healthcare. BMJ. 375:n2407.
Booth A (2022) Carbon footprint modelling of national health systems: Opportunities, challenges and recommendations. Int J Health Plann Manage. 37(4):1885-1893.
Chambrin C, de Souza S, Gariel C et al. (2023) Association Between Anesthesia Provider Education and Carbon Footprint Related to the Use of Inhaled Halogenated Anesthetics. Anesth Analg. 136(1):101-110.
Herridge MS, Azoulay É (2023) Outcomes after Critical Illness. N Engl J Med. 388(10):913-924.
Hunfeld N, Diehl JC, Timmermann M et al. (2023) Circular material flow in the intensive care unit-environmental effects and identification of hotspots. Intensive Care Med. 49(1):65-74.
Lenzen M, Malik A, Li M et al. (2020) The environmental footprint of health care: a global assessment. Lancet Planet Health. 4(7):e271-e279.
Malik A, Lenzen M, McAlister S, McGain F (2018) The carbon footprint of Australian health care. Lancet Planet Health. 2(1):e27-e35.
Martin GL, Atramont A, Mazars M et al. (2023) Days Spent at Home and Mortality After Critical Illness: A Cluster Analysis Using Nationwide Data. Chest. 163(4):826-842.
McGain F, Burnham JP, Lau R et al. (2018) The carbon footprint of treating patients with septic shock in the intensive care unit. Crit Care Resusc. 20(4):304-312.
Milner J, Turner G, Ibbetson A et al. (2023) Impact on mortality of pathways to net zero greenhouse gas emissions in England and Wales: a multisectoral modelling study. Lancet Planet Health. 7(2):e128-e136.
Muret J, Kelway C (2019) Members of the SFAR's Sustainability Group French Society of Anaesthesia; Intensive Care. Why should anaesthesiologists and intensivists care about climate change? Anaesth Crit Care Pain Med. 38(6):565-567.
NHS England and NHS Improvement (2020) Delivering a Net Zero National Health Service. Available at https://www.england.nhs.uk/greenernhs/publication/delivering-a-net-zero-national-health.
Oude Lansink-Hartgring A, Miranda DDR, Mandigers L et al. (2023) Health-related quality of life, one-year costs and economic evaluation in extracorporeal membrane oxygenation in critically ill adults. J Crit Care. 73:154215.
Pernigotti D, Stonham C, Panigone S et al. (2021) Reducing carbon footprint of inhalers: analysis of climate and clinical implications of different scenarios in five European countries. BMJ Open Respir Res. 8(1):e001071.
Prasad PA, Joshi D, Lighter J et al. (2022) Environmental footprint of regular and intensive inpatient care in a large U.S. hospital. Int J Life Cycle Assess. 27(1):38–49.
Zieleskiewicz L, Lopez A, Hraiech S et al. (2021) Bedside POCUS during ward emergencies is associated with improved diagnosis and outcome: an observational, prospective, controlled study. Crit Care. 25(1):34.










