ICU Management & Practice, ICU Volume 10 - Issue 4 - Winter 2010/2011
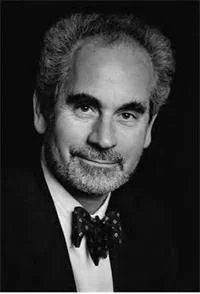
Professor of Intensive Care Medicine at the University of Birmingham, Prof. Julian Bion also has an honorary consultant appointment with the University Hospital in Birmingham. He also has a number of high-profile national and international roles in the field of intensive care, including being an Editorial Board Member of ICU Management and is a former President of the European Society of Intensive Care Medicine (ESICM).
In the second of this two-part interview with Managing Editor Sherry Scharff, Prof. Bion describes the planning and implementation of combining hospitals, and highlights the importance of fostering a family culture in even the largest of units.
SS – Can You Briefly Describe Your Department?
JB –We are in the process of moving into one of the largest Intensive Care Units in the world. I was appointed as a consultant in Intensive Care Medicine and as a Senior Lecturer in Intensive Care Medicine at the hospital and the University in 1987. In 1987, the hospital had one ICU with six beds – for the entire hospital and as a consequence of expansion and co-location of services over the following years, we finally ended up with four Intensive Care Units across two hospitals and a total of somewhere in the region of 55-60 critical care beds. More recently, approaching 65-70 ICU beds. For the last ten or so years, we have been preparing for the move into a new hospital built contiguously with the Queen Elisabeth Hospital and we finally took possession of that hospital in June (2010), and began moving patients through into the new hospital. We have two hospitals: Queen Elisabeth Hospital and Selly Oak Hospital (2.5 miles apart), with four ICUs (one in Selly Oak and three in the QE). In June, we moved all the patients formally in the Selly Oak hospital into the new hospital, together with the critically ill patients from the ICU there. We also moved the cardiac Intensive Care Unit and the post-surgical ICU from the University Hospital into the new hospital. So we moved one entire hospital and two ICUs into a new building in a matter of four days. The two ICUs with about 40 critically ill patients took about three days…
SS – It Sounds like a Logistical Nightmare…
JB – Oh it was a significant exercise, as you can imagine. But, as our Medical Director David Rosser, who is also one of our consultant intensivists said: “It’s not a matter of moving 40 critically ill patients, it’s more like moving one critically ill patient 40 times”. We set about the patient transfers very methodically and calmly, with a lot of people around- the ambulance service was fully involved of course, but also the police helped with out-riders to clear the traffic for some of the more seriously ill patients and it went very well, without remarkable incident or complication of any sort. Of course, an additional element is that we had to continue providing high quality care to the patients remaining in the units being cleared, throughout this process, as well as in the new ICU where patients were being received, and during transfer. So it did require a certain amount of attention to detail.
The severity of illness of the patients in the UK is always very significant. Many of our patients are young soldiers with military- elated injuries, some of them with appalling injuries, which I am sorry to say. Another large group of our patients, cardiac patients are very dependent- in fact one of the patients who was transferred was on extracorporeal membrane oxygenation (ECMO) and a balloon pump, so there was a lot of technical “kit” that had to accompany these patients as well. So that was the major activity during June, and later this year we will be moving the third ICU and then next year the final, fourth ICU, which is the Neuro-Intensive Care Unit and then we will all be co-located in one place. We will have about 73-75 ICU beds open in one place. We will also have another 25- 30 beds, which are not yet available, but we have established ourselves now as a 100- bed ICU, which as a single entity makes it one of the largest in the world.
SS – What is the Nurse to Patient Ratio?
JB –Well we have as a general principle in the UK, a one nurse to one patient ratio; for mechanically ventilated or patients receiving extracorporeal circuits for example on continuous dialysis. We run the ratio of 5.5 nurses per ICU bed- so this gives us something in the region of 550 nurses plus additional staff, of course, because you have to have senior staff managing the individual areas within the unit. In total, there will be about 580 nurses, once the entire enterprise is running.
SS – With Such Large Staff, there are Most Certainly some
Management Challenges to Face…?
JB –We have moved from a dispersed to a co-located model of critical care- a model including fairly large ICUs; by UK standards- these are ICUs with 15-20 critical care beds. Each had its own identity however, and staff which predominately spent much of their working lives in that location. We’ve now moved to this co-located model, which is much bigger and where the family mentality has to evolve to one much more based on a commune. This presents challenges in terms of scope and interpersonal relationships. As this is indeed a distinct cultural change, we are taking this rare opportunity to do some quality research. We have an integrated programme of quality improvement that we initiated before the move, and we are studying the impact of the move on various quality indicators. One of which, for example is the number of medical staff who are able to attend some of our professional development activities. Because when you have four ICUs across two hospitals, the one thing you can be sure of, is that you can never meet together as a group whereas, if you have everyone in one place, it’s much easier to meet as a group. So we do have the opportunity now to work together, to get together and to support each other much more effectively than we had been able to before. On the other hand, there are so many of us that it is harder to learn everyone’s names and to give the workplace a true family atmosphere. Creating that family atmosphere is quite important I think, it occurs not just through learning to work together but really, learning to live together as well and it incorporates such things as even having an annual staff party for example, which is relatively easy to do if you only have a hundred staff to organise, but when you have upwards of 600, 550 nurses, 40 consultants and roughly 40 trainees as well, it becomes quite a challenge to get that to work.
Our quality improvement activities incorporate a range of other things as well. One of the most important of which is the family and patient satisfaction survey that we have been conducting for some time now, and which is providing us with some important feedback about ways in which we can improve. Clearly the great majority of responses reveal a very high level of satisfaction, but of course this is not merely dependent on the high staff to patient ratio- which really only signals that you have very little excuse for failure, it does not guarantee affection. Although most of the time we are well rated, as you might expect, there are always areas for improvement. We always highlight any noted areas of improvement and strive to work on them. Now, with the move to a co-located model, we can continue to measure performance, monitor our progress in these areas of improvement and study whether the move has made any difference in our delivery of care.
In addition to these quality improvement activities, we have a lot of research going on which has been hampered by the dispersed model of care and which will now become a great deal easier to sustain once we are all in one location.
SS – Have You Some Wisdom to Impart to Those Entering the
Critical Care Field?
JB – Well, if I were to summarise my thoughts on critical care, I would say that it is one of the few places in the hospital where you can be a holistic practitioner, providing real quality care to the most acutely ill and susceptible patients in the hospital system.