ICU Management & Practice, ICU Volume 11 - Issue 3 - Autumn 2011
Early Enteral Nutrition in Trauma Patients
The first step in any practice change initiative involves an 'appraisal' of the research evidence to understand its inherent potential to change practice. As an example, a novel meta-analysis of early enteral nutrition in trauma is assessed.
Introduction
Up to 30% of all hospitalised patients receive care that is inconsistent with current best research evidence (Buchan 2004). Evidence-practice gaps can be reduced in a complex environment such as the intensive care unit (ICU) however the degree of practice change that can be achieved depends upon a number of factors (Doig et al. 2008; Martin et al. 2004).
Traditionally, practice change initiatives begin by identifying barriers to change (Simpson and Doig 2007) and understanding inter- and intra-professional communication patterns (Sinuff et al. 2007). Once these factors are understood an efficient practice change strategy composed of effective focussed interventions (Ex. Active reminders, audit and feedback etc) is designed (Simpson and Doig 2007). In addition to the above considerations, there are certain inherent qualities of the research evidence itself that may affect practice change.We recommend the first step in any change management initiative should involve a detailed appraisal of the research evidence to determine its inherent practice change potential. In their seminal review, Davis and Taylor- Vaisey (1997) summarised the five main qualities of research evidence that make a new treatment more likely to be translated into practice:
- The new treatment can be demonstrated to be superior to the old treatment in terms of patient benefit;
- The new treatment supports existing beliefs;
- The clinician can observe others trying the new treatment;
- The new treatment is relatively simple and;
- Parts (or all) of the new treatment can be tried by the clinician with ease.
The purpose of this paper is to focus on the intrinsic qualities of research evidence that may facilitate practice change, using early EN in trauma patients as a representative topic.
Early EN in Trauma: Evidence From a Novel Meta-Analysis
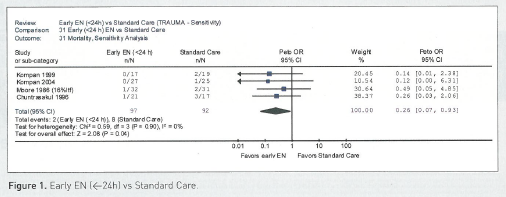
Trauma surgeons were amongst the first to conduct Randomised Controlled Trials (RCTs) investigating the benefits of early EN (Moore and Jones 1986). Although no single clinical trial has been large enough to demonstrate a significant reduction to mortality, a recently published meta-analysis of RCTs concludes that early EN significantly reduces mortality from trauma if EN is started within 24 h of injury or ICU admission (Doig et al. 2011).
The results of this novel meta-analysis are based on an extensive electronic literature search that identified 13 RCTs that evaluated timing of EN initiation after trauma. Four of these 13 clinical trials did not report patient outcomes, four evaluated the role of immune-enhanced EN products and one RCT did not start EN within 24 h of injury or ICU admission in the early group.The remaining four clinical trials evaluated the role of standard EN commenced within 24 h of injury or ICU admission and were included in the meta-analysis.
The four included RCTs enrolled a total of 189 patients. With a mortality rate of 10% in the standard care arm, a conservative meta-analytic technique appropriate for ‘sparse outcomes’ was used. Peto’s assumption free method reported mortality was significantly lower in patients receiving early EN (Figure 1; Odds Ratio = 0.26, p=0.04, I2=0). Furthermore, one included trial showed a strong reduction in pneumonia (p=0.050) and a second included trial demonstrated a strong reduction in severity of multiple organ dysfunction syndrome (MODS) (p=0.057) in patients receiving early EN. A complete critical appraisal of this meta-analysis can be found online (http://www.evidencebased.net/framesetJC.html, Accessed 17 June 2011).
Inherent Qualities of Research Evidence Relevant to Practice Change
1) The New Treatment Can be Demonstrated to be Superior to the Old Treatment in Terms of Patient Benefit.
Numerous independent sources corroborate the patient benefits attributable to early EN. For example, the authors of the Eastern Association for the Surgery of Trauma (EAST) guideline on Nutritional Support in Trauma Patients conclude that early EN leads to a reduction in MODS, intra-abdominal abscesses and pneumonia in trauma patients (Jacobs et al. 2004). Additionally, meta- analyses of clinical trials conducted in similar patient groups demonstrate early EN reduces mortality in major gastrointestinal surgery patients (Lewis et al. 2008) and in critically ill patients (Doig et al. 2009). Furthermore, an extensive review of all the evidence failed to demonstrate any proven harms arising from the provision of early EN (Heighes et al. 2009).
The new meta-analysis by Doig et al. (2011) does not need to stand alone. Significant benefits to trauma patients attributable to early EN have been documented by other reviewers and similar benefits have been reported in other patient groups. Practice change is easier to achieve when evidence of patient benefit is robust and clear.
2) The New Treatment Supports Existing Beliefs.
Today, it is accepted that early EN reverses the gut wall changes that lead to increased permeability (Goldberg et al. 2008) resulting in down-regulation of systemic immune responses and oxidative stresses which drive the incidence and severity of MODS. Any reduction in MODS would be expected to translate directly into a reduction in mortality.
3) The Clinician Can Observe Others Trying the New Treatment.
4) The New Treatment is Relatively Simple.
To make the new treatment as easy as possible to implement, a Treatment Recommendation Statement (TRS) should be prepared to summarise the new treatment for potential adopters. The TRS must be succinct but provide all key elements that a clinician requires to implement the new treatment appropriately.
The following TRS for early EN in trauma is based on the RCTs included in the meta-analysis by Doig et al. (2011): Begin standard EN within 24 h of injury or ICU admission, as soon as shock is stabilised. Stable shock can be defined as Shock Index ≤ 1 (heart rate ÷ sys- tolic blood pressure = Shock Index) or systolic blood pressure > 90 mmHg or mean blood pressure > 70 mmHg for at least one hour. Set starting rates and nutritional goals as per local ICU policy or standard practice. Gastric or post-pyloric feeding tubes may be used.
In the above example, a statement regarding shock was required since all trials included in the meta-analysis started early EN after shock was resolved. Because clinicians use slightly different end points to guide resuscitation, a working definition of ‘stable shock’ was based on criteria published in the included trials.With regards to EN starting rates and goals, because all included trials used different starting rates and goals, we chose not to stipulate specific starting rates and goals in our TRS. Preserving clinical judgement in areas where information conflicts may result in increased adherence to other key areas of the TRS (Doig et al. 2008).
The above example is over-simplified for illustrative purposes. An appropriate local process, which includes all key stakeholders, should be undertaken to generate the actual TRS used at each target site. Each target site’s TRS may differ slightly however the consideration of local factors in the generation of a simple statement will enhance implementation.
5) Parts (or all) of the new treatment can be tried by the clinician with ease.
The provision of early EN is a flexible intervention. The clinician can pick an choose the most appropriate patients for an initial trial and initial EN starting rates may be lower than the clinician usually uses. Once confidence and skills are established, more complex patients may be fed and starting rates may be increased.
Summary
Although clinicians are more likely to change practice when presented with the definitive results of a well conducted multi-centre clinical trial conducted in their own healthcare setting, a meta-analysis of smaller trials may also appropriately influence practice change (Doig et al. 2008; Perrier et al. 2011).
Inherent qualities of research evidence, such as clear patient benefits, compatibility with existing beliefs and values, “observability”, complexity, and “trialability” all contribute towards a new treatment’s up-take into practice (Davis and Taylor-Vaisey 1997). Using a novel meta-analysis demonstrating that early EN reduces mortality in trauma patients as an example, we show how appraisal from the perspective of these practice change qualities may lead to a better understanding of the potential for change. Understanding the potential for change is a necessary first step towards achieving any real change.
References:
Baue, A. E. (1975). Multiple, progressive, or sequential systems failure. A syndrome of the 1970s. Arch. Surg. 110, 779-781.
Borbas, C., Morris, N., McLaughlin, B., Asinger, R., & Gobel, F. (2000). The role of clinical opinion leaders in guideline implementation and quality improvement. Chest 118, 24S-32S.
Buchan, H. (2004). Gaps between best evidence and practice: causes for concern. Med. J. Aust. 180, S48-S49.
Davis, D. A. & Taylor-Vaisey, A. (1997). Translating guidelines into practice. A systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ. 157, 408-416.
Doig, G. S., Heighes, P. T., Simpson, F., Sweetman, E. A., & Davies, A. R. (2009). Early enteral nutrition, provided within 24 hours of injury or intensive care unit admission, significantly reduces mortality in critically ill patients: A meta-analysis of randomised controlled trials. Intensive Care Med (in press).
Doig, G. S., Heighes, P. T., Simpson, F., & Sweetman, E. A. (2011). Early enteral nutrition reduces mortality in trauma patients requiring intensive care: A meta-analysis of randomised controlled trials. Injury. 42, 50- 56.
Doig, G. S., Simpson, F., Finfer, S., Delaney, A., Davies, A. R., Mitchell, I., & Dobb, G. (2008). Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial. JAMA 300, 2731-2741.
Goldberg, R. F., Austen, W. G., Jr., Zhang, X., Munene, G., Mostafa, G., Biswas, S., McCormack, M., Eberlin, K. R., Nguyen, J. T., Tatlidede, H. S., Warren, H. S., Narisawa, S., Millan, J. L., & Hodin, R. A. (2008). Intestinal alkaline phosphatase is a gut mucosal defense factormaintained by enteral nutrition. Proc. Natl. Acad. Sci. U. S. A. 105, 3551-3556.
Heighes, P. T., Doig, G. S., Sweetman, E. A., & Simpson, F. (2009). An overview of evidence from systematic reviews evaluating early enteral nutrition in critically ill patients: more convincing evidence is needed. Anaesthesia and Intensive Care in press.
Jacobs, D. G., Jacobs, D. O., Kudsk, K. A., Moore, F. A., Oswanski, M. F., Poole, G. V., Sacks, G., Scherer, L. R., III, & Sinclair, K. E. (2004). Practice management guidelines for nutritional support of the trauma patient. J. Trauma. 57, 660-678.
Lewis, S. J., Andersen, H. K., & Thomas, S. (2008). Early Enteral Nutrition Within 24 h of Intestinal Surgery Versus Later Commencement of Feeding: A Systematic review and Meta-analysis. J. Gastrointest. Surg.
Martin, C. M., Doig, G. S., Heyland, D. K., Morrison, T., & Sibbald, W. J. (2004). Multicentre, cluster-randomized clinical trial of algorithms for critical-care enteral and parenteral therapy (ACCEPT). CMAJ. %20;170, 197-204.
Moore, E. E. & Jones, T. N. (1986). Benefits of immediate jejunostomy feeding after major abdominal trauma a prospective, randomized study. J. Trauma 26, 874-881.
Perrier, L., Mrklas, K., Shepperd, S., Dobbins, M., McKibbon, K. A., & Straus, S. E. (2011). Interventions encouraging the use of systematic reviews in clinical decision-making: a systematic review. J. Gen. Intern. Med. 26, 419-426.
Simpson, F. & Doig, G. S. (2007). The relative effectiveness of practice change interventions in overcoming common barriers to change: A survey of 14 hospitals with experience in implementing evidence-based guidelines. Journal of Evaluation in Clinical Practice 13, 709-715.
Vincent, J. L. (2005). Give your patient a fast hug (at least) once a day. Crit Care Med. 33, 1225-1229.







