HealthManagement, Volume 16 - Issue 1, 2016
Public awareness and concern about radiation safety has grown in the last few years, and concerns have been voiced about radiation dose, for example in breast imaging, across a wide range of media. Patients are concerned, as they receive conflicting, sometimes confusing information. Therefore good communication from the radiology department is essential.
How to Communicate
It is a truism, but the choice is never between communicating or not communicating, but between communicating well or badly. When the radiologist does not communicate it encourages the patient to find information on the web, for example on websites that provide a risk calculator where the patient can input data for each study (gender, age, number of exams performed, associated absorbed dose), and the software calculates the effective dose and additional cancer risk. This is very worrisome for patients, because they think, for example, that they are going for a screening examination to ensure early diagnosis of cancer, but at the same time it increases the chances of getting cancer.
When the communication is there, it can be bad, and it may even have the effect of inducing the patient not to accept the examination that is actually useful for his or her health. Radiologists have to control the “scattering” of information, by avoiding use of confusing acronyms and physical dimensions, such as absorbed, equivalent and effective dose that are familiar to professional staff, but may be confusing for the layperson.
Some departments communicate the risk associated with radiation exposure during the medical procedure by using metaphors. Instead of saying that the patient is getting so many millisieverts (mSv), which are associated with a certain increase in health problems, they propose metaphors that take into consideration risky situations that are more familiar to the patient, such as smoking or driving.
Communication Strategy
Patients do not need to be frightened. I have heard patient groups reacting to the new directive, saying, “We don’t want to know the technical details, we’re not interested in millisieverts”. Most have this reaction, because they trust doctors. They say, “I will go and have the x-ray, because you assure me that I need the examination.” They want to be assured that when they go to a hospital to have an examination, they will receive state-of-the-art service. Radiology departments have to develop an appropriate communication strategy that does not frighten or confuse the patient, and is compliant with the regulation.
Following the new directive, departments will have to record in the radiology report the radiation dose given to the patient. However, radiologists can mitigate this information, which might be threatening or incomprehensible to the patient, by adding information about the department where the examination has been performed and the procedures that are in place to ensure that variations which are not clinically justified are reduced to a minimum, thereby ensuring reproducibility, consistency and quality of all examinations.
Marketing Strategy
Radiology departments need a marketing strategy. Yes, x-rays may be dangerous, but patients have an x-ray exam because it is justified. It is useful to have decision support systems that justify the examination, and patients must be given the information that guarantees that the department is committed to quality service also in terms of radiation dose. Radiology departments should be very clear in their mission statement that in their daily practice they aim for the right diagnoses after the right exam performed at the right time with the right protocol for each patient, with respect to different ages, sex and sizes.
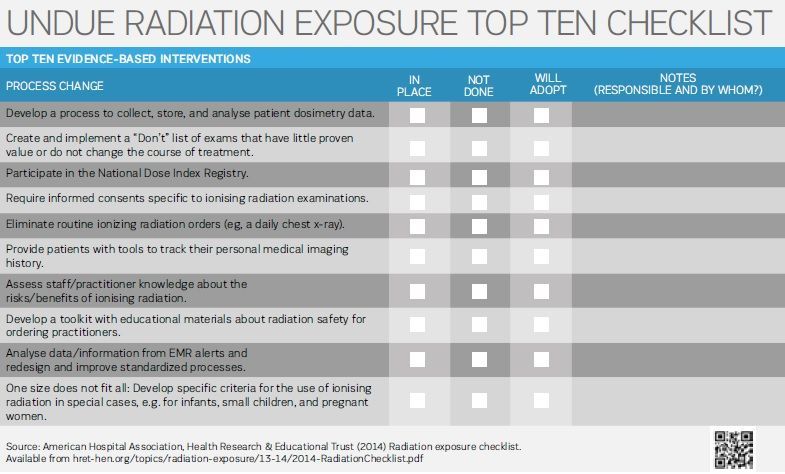
Radiology departments need to measure, and they have to systematically use the quantitative approach in order to improve, where there is a margin to improve. Departments have to show that they are performing meticulous dose tracking for the exams most frequently performed in their department, and show that variation, when it is there, is in examinations that are in principle valuable to the clinical conditions of patients that are inherently different.
Information can be more in-depth: for example, histograms are a way of benchmarking the individual examination with respect to the same type of examinations performed in a department. Histograms that show radiation dose can reassure the patient that he/she is in the group of examinations that are associated with the least amount of radiation dose. It is a subtle way of benchmarking the individual examination. Histograms can also benchmark data with other radiological groups. Patients having repeat examinations may want to have information about accumulated dose, and departments must be prepared to produce this.
Another marketing opportunity in Europe is to promote the radiology department as a Friend of EuroSafe Imaging (eurosafeimaging.org/friends-of-eurosafe). Friends of EuroSafe are committed to supporting the EuroSafe objectives:
• Promoting appropriateness;
• Maintaining radiation doses within diagnostic reference levels (DRL);
• Promoting the use of up-to-date equipment;
• Use the As Low As Reasonably Achievable (ALARA) principle;
• Improve communication with patients.
Get Ready
Radiology departments have to prepare for the implementation of the European directive by carrying out rigorous preliminary housekeeping. Marketing efforts are counter productive, if departments do not work in a very controlled way, and examinations are associated with doses that vary quite randomly. If the line of a patient’s examination is on the wrong side of the histogram without a valid clinical reason, this is not good for the department’s image. Radiology departments will be increasingly transparent, and when numbers will be on the report they have to be absolutely ready.
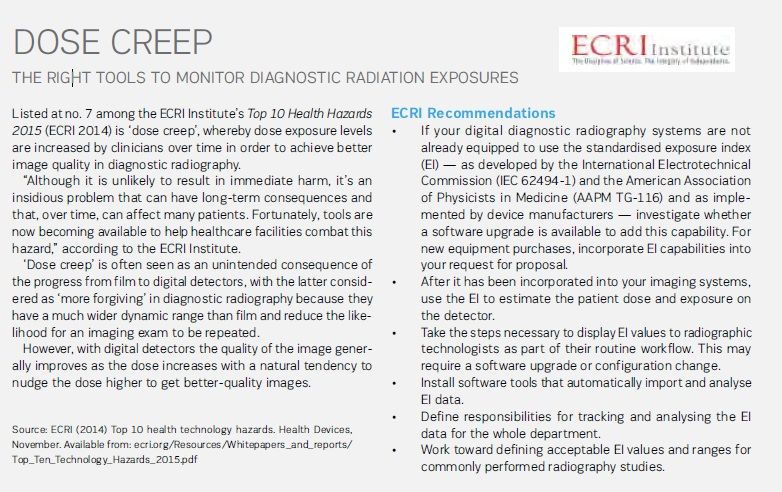
There are many commercially available radiation dose and contrast medium tracking software solutions. There is healthy competition, and the radiological community can choose the tool that is best suited for their local situation, IT infrastructure and PACS system. In my opinion, the adoption of radiation dose and contrast medium tracking software solutions is not avoidable. It is going to be very useful for fine-tuning radiological activities aiming at total quality. Departments need to make sure that variations in contrast media usage and radiation doses are all clinically justified, that there is no random deviation, and that all variations can be explained to patients. Dose tracking is needed to ensure systematic, comprehensive and shared collection of data, and the radiology department must act on it in order to improve.

In our department we started this work some time ago, and it is a lot of additional work. We established a dose team, including our chief technologist, three junior technologists, a medical physicist, an engineer and a medical student. They help me to make sure that this software provides data, and that these data do not contain errors, because sometimes the raw extracted data may need to be analysed further.
It is not easy to obtain additional help in a time of cost containment, but careful planning should be put in place before embarking on a project of radiation dose and contrast medium tracking, because this will certainly be an additional activity for already busy radiological departments.