HealthManagement, Volume 16 - Issue 1, 2016
For its fourth Deep Dive™ analysis of a particular patient safety topic, ECRI Institute Patient Safety Organization (PSO) selected care coordination issues affecting patients throughout the continuum of care. Poorly coordinated care puts patients at risk for preventable events, such as medication errors, lack of necessary follow-up care and diagnostic delays and errors. These errors and delays, as well as care gaps, can lead to repeat testing and procedures, a dissatisfying care experience and preventable patient harm, including unnecessary hospital readmissions.
Historically, the patient’s primary care provider followed
the patient’s care from the hospital to the home or to other healthcare
settings. In many instances, this no longer occurs. Hospitalists, for example,
now typically oversee patient care in the hospital setting. Outside the
hospital, patients may have multiple specialty providers in addition to their
primary care provider. Besides a family doctor, a patient may seek care from a
cardiologist, dermatologist, endocrinologist, gastroenterologist,
gynaecologist, neurologist, orthopaedist, physical therapist, rheumatologist
and others. In addition, when any of the specialists prescribes medications,
the patient may obtain them from multiple pharmacies, including mail-order
sites.
Coordinating the patient’s care among all of these various providers and across multiple care settings—from a hospital to a rehabilitation facility to the patient’s home, or from a hospital to a skilled nursing facility—is a huge challenge. on top of this challenge are various contributing factors that can impede care coordination, including patient information that is unavailable, inaccurate, not timely, or incomplete, as well as patients’ limitations in understanding their needs (e.g., understanding what medications they are taking and why, knowing whom to see for a particular care issue) so that they or a designee can safely and reliably care for themselves.
With increased attention in the public and private sectors to care coordination and its effect on patient safety, more healthcare organisations are addressing this important patient safety topic. Contributing to the discussion is the emergence of the electronic health record, which many argue will eventually help to promote the clear exchange of patient information across healthcare settings and among various healthcare providers.
Limitations
As with each Deep Dive undertaken by ECRI Institute PSO, the analysis is based on event data that is voluntarily reported by healthcare organisations; most likely, there were many more care coordination events occurring during the time period of the analysis that were not reported through the ECRI Institute PSO database. the analysed data provides a snapshot of those care coordination events that organisations chose to report and offers insights into the issues that organisations confront in coordinating a patient’s care from admission through discharge; however, because the data does not represent the universe of care coordination events occurring during the period of the analysis, no conclusions can be drawn about the frequency or severity of care coordination events and trends over time. Also, because the events for this analysis are reported by hospitals, the representation of care coordination events in our analysis leans toward those that occur in the hospital rather than those that occur in the ambulatory setting once the patient is discharged.
What ECRI Institute PSO Found
For its Deep Dive on care coordination, ECRI Institute PSO analysed 223 events reported by 38 facilities. the events were submitted to ECRI Institute PSO and its partner patient safety organisations (PSOS) over three and a half years, starting in September 2011 and ending in mid-January 2015. The analysis includes both nearmiss events (events that are detected before reaching the patient) and events that reached the patient, a few of which caused temporary or permanent harm. The reports reflect events occurring in the hospital and at or after discharge.
Among the results from the analysis, ECRI Institute PSO found the following:
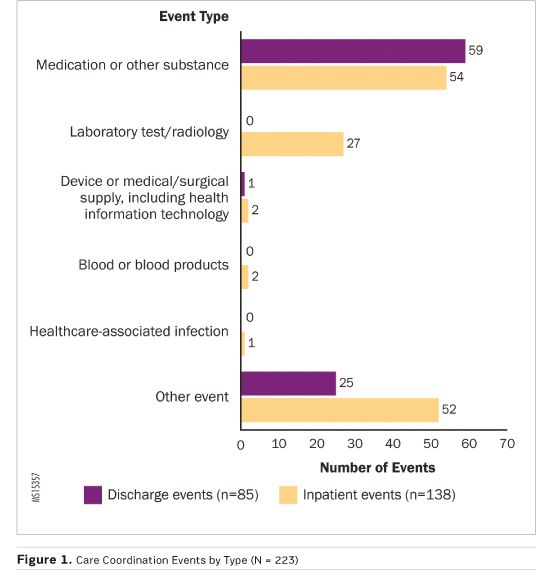
- The majority of the events (138, or 62%) involved care
coordination issues arising during the hospital stay; the remainder (85, or
38%) occurred during or after the discharge process.
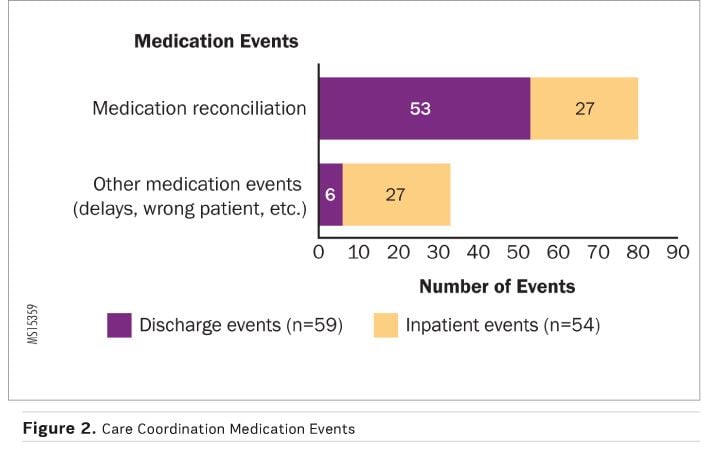
- The largest share of all the care coordination reports,
whether an inpatient-or discharge-related event, involved medications (see
Figure 1), representing 51% (113) of all analysed events; 71% (80) of all
medication events were attributed to medication reconciliation failures (see
Figure 2).
- Laboratory testing and diagnostic imaging incidents
contributed to 20% (27) of the inpatient care coordination events.
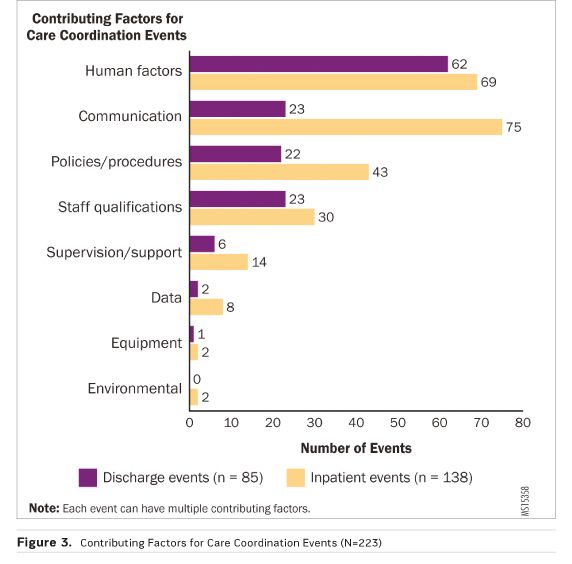
- The top four contributing factors for both inpatient and
discharge care coordination events were human factors (associated with 131
events), communication breakdowns (98 events), policies and procedures that
were either unclear or not in place (65 events), and limitations in staff
qualifications (53 events) (see Figure 3).
- Almost two of every five care coordination events in the
inpatient setting (38%, or 52) involved inadequate handoffs.
- The majority of the events for which a harm score was provided were caught before causing any harm to the patient (79 of 91 events, or 87%).
- Failure to follow up on orders for medications and
testing, leading to delays;
- Mistakes in the medication reconciliation process at
various stages of patients’ care spanning admission to discharge;
- Lack of clarification as to who is responsible for a
patient’s care, such as when a patient’s doctor goes on vacation;
- Failure to report changes in a patient’s condition to the
providers responsible for the patient’s care.
The examples illustrate the importance of ensuring that providers along the care continuum work together as a team and communicate among each other about the patients’ care.
Improvements in care coordination depend on providers in all healthcare settings recognising their shared responsibility to facilitate seamless patient transitions along the care continuum. ECRI Institute PSO's Deep Dive report reviews the effect that issues such as medication reconciliation, discharge planning, care transitions, patient engagement, and more can have on care coordination along the healthcare continuum. The report provides recommendations to address these issues and, in turn, to improve care coordination.
Key Recommendations
Leadership
- Provide support for the organisation’s care coordination
improvement initiatives to mobilise the many stakeholders who contribute to the
efforts and to provide the necessary resources and staff to support the
initiatives.
- Solicit feedback from patients and their family members
about their care experiences.
- Consider the business case for care coordination
initiatives (i.e., quantify the cost savings from specific risk mitigation
strategies, such as medication reconciliation).
- Assign a multidisciplinary team responsible for
identifying improvement projects and led by a project champion to oversee the
team’s day-to-day work.
- Support care coordination improvement strategies that
incorporate a hierarchy of error reduction techniques.
Event Reporting, Identification and Analysis
- Develop a safety culture, supported by non-punitive event
reporting policies, in which frontline staff, clinicians, and others recognise
the value of reporting events and near misses associated with care
coordination.
- Learn to evaluate events from the perspective of care coordination
and to consider how different event types, such as medication or testing
errors, can involve care coordination.
- Look beyond the data in the organisation’s event reporting
programmes to other data sources (eg, case management reports, patient surveys
and complaints, trigger tools, reports from other organisations) to evaluate
care coordination processes.
- Consider ways to encourage reporting and feedback about
the discharge process from physician practices and other ambulatory settings
and from postacute care facilities.
- Consider using the Agency for Healthcare Research and Quality’s readmissions Common Format, once it is finalised, to
evaluate readmissions and identify prevention strategies.
Medication Reconciliation
- Adopt a systematic and comprehensive process for
medication reconciliation, and conduct medication reconciliation each time a
patient transitions to a new level of care along the continuum of care.
- Identify a medication reconciliation process that is
suited to the organisation’s needs; refer to the numerous resources available
to assist organisations with medication reconciliation.
Communication and Information Transfer
- Adopt practices—such as handoffs, briefings and huddles,
and multidisciplinary rounding—that simplify and standardise communication and
enhance patient safety by reducing communication breakdowns.
- Recognise that effective care transitions between
hospitals and postacute care providers are a two-way responsibility.
- Develop a standardised transfer form to communicate the
necessary information that a postacute care provider will need when a patient
is transferred from the hospital to the postacute setting.
- Foster collaborative strategies (eg, regular meetings at
provider sites, discussion about suboptimal transfers) to build relationships
of mutual trust between hospitals and postacute care providers.
Discharge Planning
- Develop a comprehensive approach to discharge planning to
ensure all patients are appropriately discharged with the provision of adequate
post discharge services.
- Identify personnel (eg, nurses, case managers, social
workers, nurse navigators) who will assist patients and their caregivers in
navigating the discharge process.
- Engage patients and their family members in discharge planning
and education.
- Conduct follow-up visits (eg, by telephone) with the
patient after discharge to address any questions and promote compliance with
the discharge plan.
Health Information Technology
- Recognise health information technology’s (it) promise in
improving care coordination and promote the efficient exchange of electronic
patient information, but pay careful attention to system planning,
implementation and ongoing use to ensure the technology’s safe and appropriate
use.
- Perform data analytics on patient data collected by health
it systems to promote better care coordination and identification of lapses in
patient care.
- Promote patients’ electronic access to their healthcare
data through patient portals to enhance partnerships between providers and
patients, leading to improved care coordination.
Patient and Caregiver Education and Engagement
- Involve patients and their caregivers with shared decision-making
by patients and providers.
- Include the patient in developing their plan of care.
- Ensure that patients understand the information given to
them regarding their care.
- Target patient education to meet the individual’s needs.
Performance Improvement
- Conduct a proactive risk analysis to identify performance
gaps in the organisation’s approach to care coordination processes, such as the
medication reconciliation process.
- Identify metrics to measure the effectiveness of care
coordination activities and to identify additional areas of performance
improvement.
- Select hospital performance goals for care coordination
that are specific and measurable.
- Ensure regular review of the data by the organisation’s
quality or performance improvement committee.
- Provide reports to
senior leaders on the effectiveness of care coordination initiatives to sustain
the organisation’s commitment in this area.
Share, Learn, Protect
The patient safety and Quality improvement act of 2005 created a framework for healthcare providers to improve patient safety by sharing data with PSOS that provide analysis and feedback regarding patient safety matters in a protected legal environment. Additionally, PSOS can collect the information in a standardised format in order to aggregate the data and learn from it.
by looking at the information from the shared events, ECRI Institute PSO’s deep dive analysis of care coordination identifies the many ways that inadequate care transitions can jeopardise patient safety by causing medication errors, wrong treatments, diagnostic delays, poorly managed transitions to postacute care settings and more.
Many of the events reported to ECRI Institute PSO and its collaborating organisations describe the challenges to care coordination within the hospital, at discharge and during transitions from the hospital to other settings. Fortunately, numerous public-and private-sector initiatives are emerging to address these challenges. Many of these strategies—such as reengineered discharge planning, comprehensive medication reconciliation, collaborative models of care transitions, patient engagement at discharge and carefully designed health it systems to support health information exchange—are discussed in ECRI Institute PSO’s report.
As healthcare is increasingly delivered outside the hospital, hospitals must work with providers along the continuum of care to identify the care coordination challenges that arise beyond the hospital in ambulatory settings and in postacute care. Identifying these issues and finding solutions to this vexing patient safety issue requires that providers across the continuum of care abandon siloed approaches to patient care and support smooth and effective care delivery and transitions.
Those organisations leading the charge are already removing many of the barriers to care coordination identified in this deep dive analysis. ECRI Institute PSO encourages all healthcare organisations to consider the recommendations of this report and to support the sharing of patient information across the care continuum in order to deliver safe, high-quality patient care.*
* For more information about ECRI Institute PSO’s deep dive
reports and toolkits, contact ECRI Institute at [email protected]. The reports
are also available for sale from ECRI Institute’s online store at
eshop.ecri.org.
Acknowledgements
ECRI Institute PSO thanks its collaborating member organisations and partner PSOs for sharing their care coordination–related events for this Deep Dive report. Over the course of four Deep Dive projects on various topics, participating healthcare organisations continue to learn multiple patient safety lessons from the aggregated analysis of shared events. ECRI Institute PSO encourages its members to review the findings from this report and to enlist a multidisciplinary team of representatives from senior leadership, clinical departments and care settings, medical staff, pharmacy, case management, social work, discharge planning, information technology, risk management, patient safety, quality improvement and other areas to discuss the applicability of the findings to the organisation. Further, as this analysis demonstrates, organisations must reach beyond their four walls of the hospital setting to other providers in their communities and collaborate to develop better systems for care coordination. Change will happen when the healthcare community is united in its journey to identify strategies to support improved care coordination activities and transitions. In addition to the many individuals at ECRI Institute who contributed to this report, ECRI Institute PSO acknowledges the following individuals for their insights about this report:
- Doug Bonacum, CPPS, Vice President, Quality, Safety, and Resource Management, Kaiser Permanente (Oakland, California)
- Margaret P. Chu, RN, BSN, MPA, CCM, CPHQ, Director, Case Management Society of America (CMSA); Executive Director, CMSA Long Island Chapter; President, MPC & Associates (East Williston, New York)
- Christina Michalek, BSc Pharm, RPh, FASHP, Medication Safety Specialist, Institute for Safe Medication Practices (Horsham, Pennsylvania)
- Heidi Porter, RT, BSC, MAE, Director of Quality Management, Wheeling Hospital (Wheeling, West Virginia)
- Richard G. Roberts, MD, JD, Professor of Family Medicine, University of Wisconsin School of Medicine and Public Health (Madison)
- Debra Zanath, RN, BSN, JD, Esq., Ohio Patient Safety Institute PSO Consultant
About ECRI
ECRI Institute, a nonprofit organisation, dedicates itself to bringing the discipline of applied scientific research in healthcare to uncover he best approaches to improving patient care. As pioneers in this science for nearly 45 years, ECRI Institute marries experience and independence with the objectivity of evidence-based research.
ECRI’s focus is medical device technology, healthcare risk and quality management, and health technology assessment. It provides information services and technical assistance to more than 5,000 hospitals, healthcare organisations, ministries of health, government and planning agencies, voluntary sector organisations and accrediting agencies worldwide. Its databases (over 30), publications, information services and technical assistance services set the standard for the healthcare community.
More than 5,000 healthcare organisations worldwide rely on ECRI Institute’s expertise in patient safety improvement, risk and quality management, healthcare processes, devices, procedures and drug technology. ECRI Institute is one of only a handful of organisations designated as both a Collaborating Centre of the World Health Organization and an evidence-based practice centre by the US Agency for healthcare research and quality in Europe. For more information, visit www.ecri.org.uk


