HealthManagement, Volume 22 - Issue 4, 2022
Benefits of Artificial Intelligence in Healthcare
In an age of Artificial Intelligence (AI) and Internet of Things (IoT) in healthcare, it is impossible that there is no communication with each other. AI in healthcare gives us, as species, the opportunity to start measuring on and communicating of the whole thing.
The organism, and the organism environment; moving what we can see out of the realm of the conceptualised abstract to the realm of the physical. What we can measure, what we opinionate on, and what we can communicate and strategise on.
AI and IoT in healthcare reform, therefore, enables us to reach a new different level of magnification which can observe and measure our internal and external surrounding. In other words, we can learn to zoom in, or zoom out.
Around the globe, the global and regional health ecosystems can find great value in the adoption of Innovation and AI-driven health strategy-based solutions for patients and physicians, together.
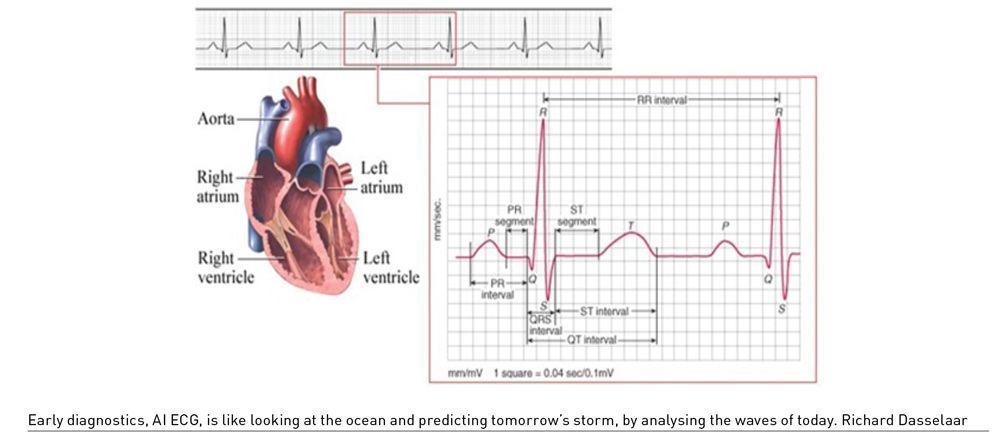
The pragmatic benefits of AI are ominous. AI, at its core, is a tool for executing efficiency. The pragmatic, or practical implications of AI and IoT in healthcare are better outcomes for patient and their caregivers on the factuals (actual facts) that matter most to us - delivered real-time, or, ahead of time, in the case of early diagnostic or prognostic artificial intelligence.
Realising the Benefits of Artificial Intelligence
What exactly does “better outcomes for patient and caregiver” mean? It is a great question but is it dependent on the image of objectives of the ecosystem, or the image we as a society place of the individual patient or caregiver?
As a strategist, and innovation leader in the realm of digital transformation by logic strategy design and strategy delivery, I measure the outcomes of what we like to achieve, based on logic, and meaningful datapoints – those being improving health outcome and/or lowering costs.
In the case of AI, the most obvious realised benefits in the short term are cost savings and freeing up the valuable time of medical personnel, which is useful as the demand for medical personnel outperforms its availability. Secondly the medical potential of AI is improving health outcome by means of AI-driven, prognostic, early diagnostic or diagnostic capabilities.
The best step from ideation to strategic implementation is the value-based healthcare strategies coined by Prof Ing. Michael Porter (2006), Prof Elisabeth Teisbergand and Prof Robert Kaplan, It is most suitable for implementing Innovation and AI-driven health strategy on global or regional health ecosystem, level, population health, or individual health – zero distance to user.
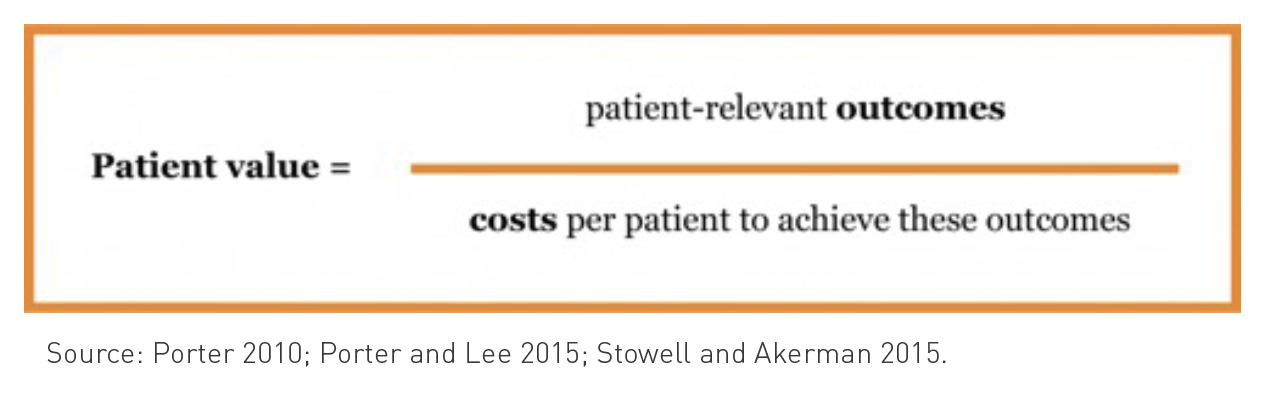
The benefits of AI in healthcare seem to help facilitate next to technological advancement, which is by design reactive to an AI and human centred driven proactive digital healthcare eco system where personalised digital self-care intervention is scalable and defined per measurable logic element and refinement per clinical area and its cost. It is based on outcomes and cost.
Therefore, logic digital health transformation leadership, “At Scale” starts with digital AI-driven (AI-ECG) self-care cardiology, as it is the costliest in both finance and human health. The theory being, the sooner we are able to recognise a disease, the lower the cost to care treating this specific disease.
Let’s illustrate with an example. A stent (stenting or shunting) is easier to place in an outpatient facility, and at lower cost than open heart (robotic & AI navigated) heart surgery within an academic hospital.
If we zoom out again and focus on the digital transformation and AI strategies for global and regional care ecosystems, we will finally find an AI strategy where all nations, both affluent and otherwise can unite behind. It can deliver in culture relevant capabilities and leverage something the World Health Organization (WHO) calls “Universal Global Health Systems”. It can help us realise our dream of an inclusive, egalitarian society.
Impact of Artificial Intelligence on Healthcare Staff
Artificial Intelligence will augment medical staff, or, in some instances replace it since there is limited need after automation to let people do repetitive tasks in a system where we have shortage of skilled medicals professionals. Or, in case of underserved or rural regions of our world, AI can augment, by providing first line of defense via digital self-care intervention.
Limitations of Artificial Intelligence
The only limitation I see at this moment is people’s urge to limit innovation (club it to death) under the flag of safety and regulation. We should consider AI as a non-invasive tool, which delivers or excludes false negatives, or false positives. We should focus on giving our physicians and healthcare teams - highly respected and esteemed professionals - with the tools and capacities to treat their patients within their clinical domain, with the tools and mentality as a fighter pilot in the cockpit, having all kinds of precision diagnostic sensors. This would make the patient more educated, and the doctor, in control of the possibility to have a 10,000 feet perspective and zoom in on the finesse of advanced heartcare, and discuss the data driven outcomes with a team of medical experts by communicating. This is simply because in an age of AI and IoT in healthcare, it is impossible that there is no communication with each other.
Conflict of Interest
None.
References:
Porter ME, Lee TH (2015) Why strategy matters now. N Engl J Med. 30;372(18):1681-4.
Porter ME (2010) What is value in health care? N Engl J Med. 23;363(26):2477-81.
Porter ME (2006) Redefining Health Care Creating Value-based Competition on Results. Presentation, National Association of Chain Drug Stores Annual Meeting.
Stowell C, Akerman C (2015) Better Value in Health Care Requires Focusing on Outcomes. Harvard Business Review. Available from https://hbr.org/2015/09/better-value-in-health-care-requires-focusing-on-outcomes



