HealthManagement, Volume 23 - Issue 2, 2023
Generative AI imaging has emerged as a powerful tool in radiology, allowing for the creation of highly detailed bio-models that can assist in diagnosis and treatment planning. Generative AI algorithms can generate 3D models of organs, tissues, and other structures with unprecedented accuracy and speed.
This technology thus has the potential to revolutionise the field of radiology, enabling more accurate and personalised medical care, including synthetic data for training or creating specific understandable bio-models, and clinical information to patients, enhancing health literacy and automating the generation of anamnesis and clinical notes. However, it also raises many ethical, regulatory, legal and philosophical questions that need to be solved before being ready for wide adoption in healthcare.
Key Points
- Generative AI will have a role in radiology departments at different levels: professional-patient communications, quality and processes, as well as in the generation of medical imaging.
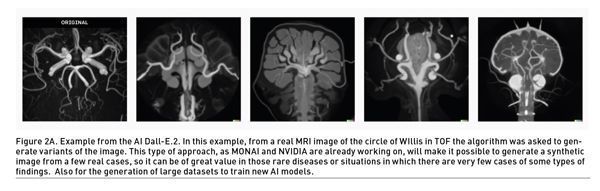
- Generative AI Imaging can have multiple uses, an example of which synthetic imaging generation for diagnosis. On the one hand, enhancing or accelerating the radiological images, but also as an aid to augment AI training databanks for rare or data-poor diseases.
- Medical imaging biomodels currently have multiple applications: surgical planning, student training, and improved communication with patients. Generative AI imaging tools will facilitate accessibility and speed of implementation in these scenarios.
- However, there are still many technical, usability, regulatory and ethical limitations to the implementation of these solutions. We must begin to collate experiences, research, and test the applicability in order to extend its use in an appropriate manner.
What Is a Generative Image AI? And, How Can It Be Applied and What Effect Will It Have in Imaging?
Deep learning has revolutionised the field of artificial intelligence (AI) by enabling machines to learn from large amounts of data and perform complex tasks based on them. One of the most exciting applications of deep learning is in the field of generative models. Generative models are deep learning models that can generate realistic images, videos and audio. These models have a wide range of applications in healthcare, including imaging.
Generative Image AI is a type of artificial intelligence that can generate images that are similar to real-world images or those used to train the algorithm. These models use deep learning algorithms to analyse and understand the patterns and features of real-world images, and then use that knowledge to generate new images that are similar in appearance.
There are several types of generative image AI models, including Generative Adversarial Networks (GANs), Variational Autoencoders (VAEs), and Autoencoders.
GANs are a popular type of generative image AI model that consists of two neural networks: a generator network and a discriminator network. The generator network generates synthetic images, while the discriminator network attempts to distinguish between the synthetic and real images. The two networks are trained together in an adversarial manner, where the generator tries to fool the discriminator and the discriminator tries to correctly classify the synthetic and real images. GANs have a wide range of applications in radiology, including image segmentation, image synthesis and image de-noising. Image segmentation is the process of dividing an image into multiple regions or segments. GANs can be used to segment medical images such as MRI scans, CT scans and X-rays. GANs can also be useful for synthesising medical images that are difficult to acquire, such as rare diseases or anatomical variations. GANs can also be used to de-noise medical images, which can improve the accuracy of diagnosis and treatment planning. One of the major challenges in radiology is the scarcity of labeled data. Labeled data is data that has been manually labeled by a radiologist or a medical expert. GANs can be used to generate synthetic data that can augment the labeled data and improve the accuracy of the models. This can also help reduce the time and cost involved in acquiring labeled data.
VAEs are another type of generative image AI model that uses an encoder-decoder architecture to generate images. The encoder network maps the input image to a low-dimensional latent space representation, while the decoder network maps the latent space representation back to the input image. The VAE is trained to learn the distribution of the input data in the latent space representation, and to generate new samples from that distribution.
Autoencoders are a simpler type of generative image AI model that use a single neural network to learn a compressed representation of the input image. The compressed representation can then be used to generate new images that are similar to the original image. The goal of the VAE is to learn a latent space representation that captures the underlying distribution of the input data. This latent space representation can be used for a variety of tasks, such as image generation, data augmentation, and classification.
One application of VAEs in medical imaging is image segmentation. Image segmentation is the process of dividing an image into different regions or segments, each of which corresponds to a different anatomical structure. VAEs can be used to learn a low-dimensional representation of the imaging data that captures the underlying distribution of the anatomical structures in the image. This low-dimensional representation can then be used to perform image segmentation.
Generative Imaging Algorithms Will Help in the Creation of Synthetic Radiological Images but also to Design New Bio-Models
A quick history about Generative AI:
Generative AI has become a trend since its first launch on November 22nd 2022, creating high expectations about a long-awaited potential of AI real use. ChatGPT gained one million users in its first week after launch and reached the milestone of 100 million users in the 2 months, surpassing all known digital solutions so far.
The use of Generative Artificial Intelligence (AI) in healthcare has the potential to revolutionise the management of health and help on diagnosis and treatment. One area where this technology has already shown promise is in the creation of synthetic imaging such as 3D bio-models and radiological images.
By improving accuracy, reducing costs, and streamlining processes, this technology can help healthcare providers deliver better care to their patients. Its earlier adopters are already reporting first evidence of the potential impact. For instance, Dr. Isaac Kohane, a computer scientist at Harvard and a physician in his book, “The AI Revolution in Medicine” (Lee et al. 2023) applied Chat GPT-4 to a US medical licensing exam, which the algorithm passed, being able to diagnose a real-life case of a congenital adrenal hyperplasia based on data from the physical exam, as well as some information from an ultrasound and hormone levels.
This is a rare disease affecting 1 in 100,000 newborns.
In another example, researchers from the Massachusetts General Hospital (MGH) and AnsibleHealth, published in a recent study (Kung et al. 2023) that Chat GPT-4 can pass the United States Medical Licensing Exam (USMLE) without clinician input with a score of 60% accuracy, exceeding the passing score on USMLE by over 20 points. These results are in line with similar research done by Nori et al (2023) and Freedman et al (2023).
However, there are also challenges associated with the use of generative AI in healthcare. Privacy concerns and the potential for bias are just two examples. As with any new technology, it is important to approach generative AI with caution and to address these issues as they arise.
Nonetheless, generative AI represents a significant opportunity for healthcare providers to improve patient outcomes and advance the field of medicine.
What Is the Potential Role of Generative AI in the Medical Imaging Departments?
This potential to transform the practice of radiology may occur in several ways in general workplace management, exam reporting and last but not least, enhancing the imaging itself.
Here are some actual practice examples:
- Automating Repetitive Tasks: Radiologists spend a significant amount of time performing routine tasks such as locating and measuring abnormalities in medical images. Generative AI can automate these tasks, reducing the time and effort required by radiologists and enabling them to focus on more complex cases.
- Facilitating Remote Consultations: Generative AI can enable radiologists to provide remote consultations and second opinions in routine cases, automating the process to give a first answer even when they are not physically present with the patient. This can be particularly useful in situations where there is a shortage of radiologists or when patients are located in remote or underserved areas.
- Extracting structured information from unstructured radiology reports for research or secondary use of data.
- Translating radiology reports into a layman version so that patients better understand them.

Focusing on Imaging Generative AI, the main potential roles are:
- Improving Diagnostic Accuracy: Generative AI can improve the accuracy of radiological diagnoses by providing radiologists with additional information and insights. For example, AI algorithms can analyse large datasets of medical images to identify patterns and trends that may not be immediately apparent to imager’s eyes.
- Enhancing Image Analysis: Generative AI, combined with other image processing and AI techniques, can be used to enhance the analysis of medical images, enabling radiologists to identify subtle changes that may be difficult to detect with the naked eye. For example, AI algorithms can be trained to identify the early signs of disease processes, such as (malignant) tumors or degenerative conditions. Generative AI models can be used to ‘clean up’ medical images by removing noise or artifacts. For example, generative models can be trained to remove noise from medical images such as MRI or CT scans, making them easier to interpret and analyse.
- Medical imaging synthesis with generative AI algorithms and other artificial intelligence techniques could generate synthetic medical images that are visually realistic and clinically relevant and that can resemble real patients images in different acquisition techniques such as US, MRI, and CT scans. The capacity of generating infinite newly created data can enable the training and validation of AI algorithms, reducing the need for live patient data, and enabling the generation of diverse and customizable medical images for specific research or educational needs.
- Automated Diagnosis: Generative AI models can be trained to analyse medical images and provide automated diagnosis. For example, generative models can be trained to detect abnormalities in any and all medical images, and provide a diagnosis based on the type and severity of the abnormality.
- Image Segmentation: Generative AI models can be trained to segment medical images into different regions based on the structures and tissues present. This can be useful in identifying and analysing specific structures or tissues in medical images such as the brain or lungs.
Personalising Treatment Plans: Generative AI can help radiologists develop personalised treatment plans based on a patient’s individual characteristics and medical history. For example, AI algorithms can analyse medical images to identify the most effective treatment options for a particular patient based on factors such as age, gender, and medical history. Generative AI models can be also used to simulate the effects of different treatment options on medical images. For example, generative models can be trained to simulate the effects of radiation therapy on a patient’s medical images, allowing imagers to optimise treatment plans.
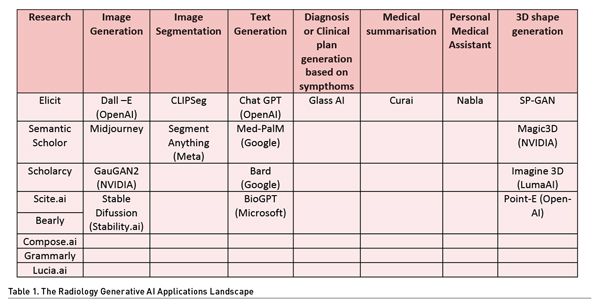
Various Generative AI algorithms are today available that could be of potential use in the field of radiology. Table 1 shows the Radiology Generative AI Applications Landscape:
In summary, the use of generative AI in radiology has the potential to improve diagnostic accuracy, increase efficiency, and enhance patient care. However, it is important to note that AI should not replace the expertise of radiologists but rather complement and support their work becoming a useful tool.
The Importance of Human Imaging Bio-Models in Healthcare
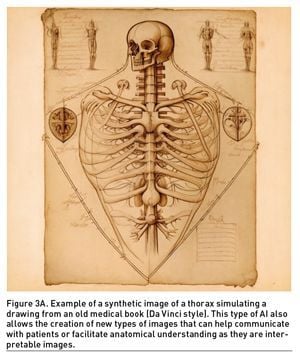
The transition from hand-drawn anatomical models to digital models and eventually to AI-generated models has been a gradual process driven by advancements in technology. Before delving into the role of AI-synthesised image, we must explain the healthcare value of imaging bio-models.
Hand-drawn anatomical models have been used for centuries to teach anatomy and physiology. With the advent of digital technology, these models were digitised and rendered in 3D, allowing for more interactive and realistic visualisations. However, creating accurate and detailed 3D models can be a time-consuming and expensive process. With the development of AI, generative models can now be trained on large datasets of medical images to generate highly detailed and realistic anatomical models. These models can be generated much faster and with greater accuracy than traditional methods, and can be used for a variety of applications in healthcare, including diagnosis, treatment planning, and medical education.
A. What Are the Main Applications of Bio-Models and Medical Imaging Design?
These bio-models, whether inspired by reality, created through traditional design methods, or specially extracted from radiological (medical) images, allow for improvements in the field of medicine. Furthermore, recently, thanks to 3D imaging technologies (whether through automatic projections and renderings or through 3D models for visualisation in augmented or virtual reality), the value of bio-models has been further demonstrated.
- Improved Diagnostic Accuracy: Medical image design can help healthcare professionals visualise and understand complex medical conditions, resulting in improved diagnostic accuracy. Accurate diagnosis is essential for effective treatment planning and can lead to better patient outcomes.
- Disease Image Pattern Study: Finally, 3D imaging can be used to study the patterns of disease in patients. By analysing 3D images of organs and tissues, medical professionals can identify patterns of disease progression and develop new treatment strategies. For example, 3D imaging can be used to study the growth patterns of tumors, identify areas of ischemia in the heart, or detect early signs of Alzheimer disease in the brain.
- Treatment Planning: Medical image design can be used to simulate the effects of different treatments, allowing healthcare professionals to develop customised treatment plans for individual patients. This can help ensure that patients receive the most appropriate and effective treatments.
- Education: Medical image design can be used to create educational materials for healthcare professionals and patients. For example, medical animations can help explain complex medical concepts and procedures, while medical illustrations can help visualise the structures and functions of the human body. 3D images provide an excellent tool for teaching complex anatomical structures and help students to understand the spatial relationships between different anatomical regions. Furthermore, 3D imaging can be used to simulate surgical procedures, which can provide students with valuable experience before performing actual surgeries. By providing a realistic and immersive experience, 3D imaging can help to improve the quality of medical education.
- Reduced Risk: Medical image design can be used to simulate medical procedures, allowing healthcare professionals to identify potential risks and develop strategies for mitigating those risks. This can help reduce the likelihood of complications and improve patient safety. Geometric Understanding of Complex Anatomy: 3D imaging also provides a more accurate and detailed view of complex anatomical structures. By creating 3D models of structures such as the brain, heart, and spine, medical professionals can gain a better understanding of their shape, size, and orientation. This information can be used to plan surgeries and treatments more effectively, leading to improved patient outcomes. Additionally, 3D imaging can also be used to create custom prosthetics and implants that are tailored to the patient’s unique anatomy.
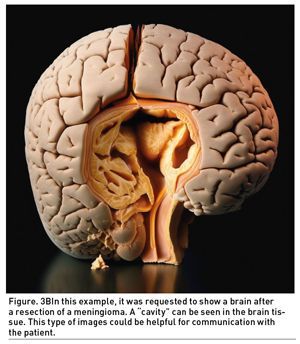
- Improved Patient Communication: Medical image design can help improve communication between healthcare professionals and patients. Visual aids such as medical animations and illustrations can help patients better understand their medical conditions and treatment options, resulting in more informed decision-making and better patient outcomes. One of the main advantages of 3D imaging in medicine is the ability to improve patient education. 3D images provide patients with a more accurate and comprehensive view of their anatomy and medical condition. Patients can easily visualise their condition and understand the nature of their disease or injury, which can lead to better patient compliance and satisfaction. Furthermore, 3D imaging can also help patients to understand the surgical procedure, and this can reduce anxiety and improve outcomes.
 |  |

B. How Can Imaging Generative AI Enhance the Imaging Bio-models?
Here are some of the possibilities of using synthetic medical imaging created with generative AI:
- Augmenting Real Medical Images: Synthetic medical images generated by generative AI can be used to augment real medical images. For example, synthetic images can be used to enhance the resolution of real images, to create additional images of organs or structures that are difficult to visualise with current imaging techniques, or to simulate the effects of different treatment options on medical images.
- Data Augmentation: Synthetic medical images can be used to augment datasets for machine learning models. This is particularly useful when the amount of real medical image data is limited or when the available data is imbalanced.
- Medical Image Analysis: Synthetic medical images can be used to train and test algorithms used for medical image analysis. Generative AI can be used to create synthetic images that are similar to real images, but with known characteristics such as specific abnormalities or tissue types. This can help in the development and testing of algorithms used for medical image analysis.
- Research: Synthetic medical images can be used in medical research to simulate disease progression or treatment effects. For example, generative AI can be used to simulate the progression of Alzheimer disease or the effects of chemotherapy on tumors.
- Education: Synthetic medical images can be used in medical education to provide students with additional images for study and practice. Generative AI can be used to create synthetic images that are similar to real images, but with known characteristics such as specific abnormalities or tissue types. These images can be used to teach students about specific diseases or conditions.
Overall, the possibilities of using synthetic medical imaging created with generative AI are vast and have the potential to greatly enhance medical research, diagnosis, and treatment planning. However, it is important to note that these images must be thoroughly validated and tested before they can be used in clinical settings.
Generative AI also Has Several Limitations:
While ChatGPT and other generative AI systems create great expectations for the long-awaited democratisation of AI in many sectors, including healthcare, they also raise many ethical, regulatory, legal and philosophical issues that need to be resolved before widespread adoption. In fact, some of the earliest adopters of the technology since the launch of ChatGPT in November 2022, already started to report first issues. As an example, according to The Economist Korea (2023), on March 20th, the Samsung’s Korea-based semiconductor business reported 3 data leakage accidents occurred within Engineers of the semiconductor plants: The developers sent confidential lines of code to ChatGPT on three separate occasions, which the AI chatbot leveraged as training data for future public responses. This act, automatically supposed a leaking corporate secret that could be included in the chatbot’s future responses as it is stated by the OpenAI user guide warning users: “We are not able to delete specific prompts from your history. Please don’t share any sensitive information in your conversations.” The system uses all questions and text submitted to it as training data. Moreover, on 31st May 2023, Italy’s data protection agency announced the blockage use of ChatGPT within the country while studying the potential violation of GDPR compliance (The Italian Data Protection Authority 2023).
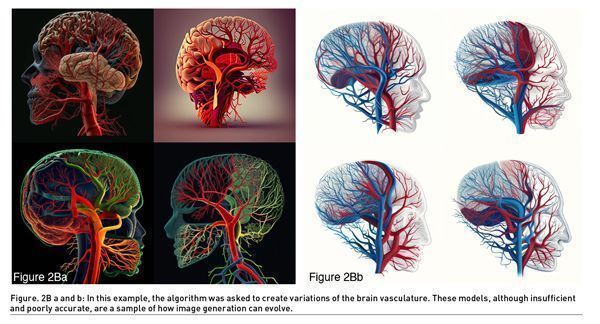
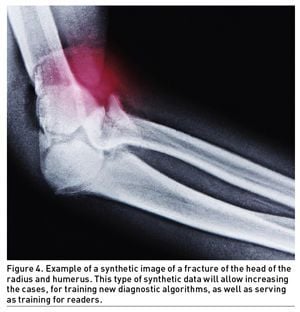
Above mentioned examples, poses a need for regulation and reflection on the potential uses of these new technologies, and this is also the case for the use of biomodels. Today, as can be seen in the following examples, photo-realistic images generated by generative AI still have a moderate intrinsic error that makes the results unrealistic, needing to be validated by an expert. This highlights the importance of quality control. However, considering the main nature of continuous learning of generative AI algorithms, we will soon be able to have re-trained and improved algorithms focused on medical imaging capable of having highly accurate image results.
In addition to those “model” generated problems, there are other limitations of image generative AI:
- Limited Information: Generative AI models are trained on specific datasets and may not generalise well to new, unseen data. This means that the generated images may not accurately represent real-world images and may contain artifacts or distortions. Actual generative AI models may lack anatomical precision because they are trained on large publicly available datasets, rather than on specific datasets of medical images with a quality control with a deep understanding of human anatomy. For example, a generative AI model that generates images of people may be trained on a large dataset of photographs, but it may not have a comprehensive understanding of the underlying structure of the human body. Additionally, generative AI models are typically designed to generate output quickly and efficiently, which can lead to simplifications and inaccuracies.
- Computational Requirements: Generative AI models require significant computational resources to train and generate images. This can make it challenging to apply these models in real-time or in resource-constrained environments. However, ongoing studies focus on improving the computational efficiency, which opens the door that in a few years it will not be unusual to have customised and private generative AI algorithms trained for specific tasks.
- Data Bias: Generative AI models can be biased if the training data is biased. For example, if the training dataset contains mostly images of a specific demographic group, the generated images may not be representative of the general population. This leads to potential gender, ethnic, racial and intrinsic imbalances due to the entry training data. As with any AI algorithm, quality control and preparation of the input data is important.
- Limited Control: Generative AI models are often difficult to control, meaning that the generated images may not align with specific requirements or desired features. This can be particularly challenging in medical applications where specific features or abnormalities need to be highlighted.
- Ethical Considerations: Generative AI models can be used to create realistic images of people or objects that do not exist in the real world or that resemble publicly known individuals. This raises ethical concerns around the potential misuse of these images, such as the creation of deepfakes or other forms of digital manipulation.
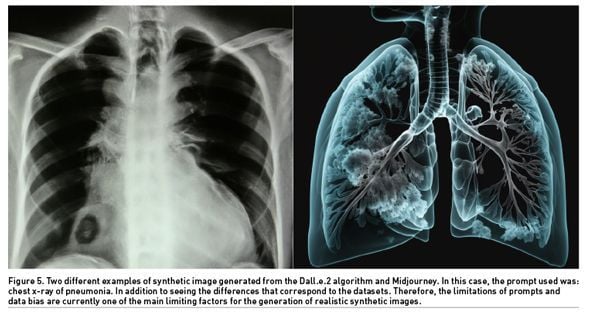
Prompts are crucial in generative AI because they provide a starting point for the model to generate new content. A prompt is a piece of text or input that the generative AI model uses to generate new output, such as a story, a poem, a piece of music, or even an image. Without prompts, the generative AI model would not know where to start or what kind of output to generate. Prompts help to guide the model and give it context and direction. By providing a prompt, the user can influence the output of the model and steer it in a particular direction. Prompts can also be used to fine-tune generative AI models for specific tasks. But, when prompts are not used correctly with generative AI, several problems can arise. Without clear and appropriate prompts, the model may generate irrelevant or nonsensical output, or it may simply repeat the same output repeatedly. In some cases, the output may be offensive or harmful, particularly if the model has been trained on biased or inappropriate data. Additionally, without careful monitoring and selection of prompts, the model may become overfit to a specific set of prompts, limiting its ability to generate diverse and novel output.
In response to the accelerated adoption of these new tools, the European Parliament issued on 23 March 2023 a communication on Generative AI and ChatGPT stating that: “The recent launches of artificial intelligence (AI) tools, and the development of general-purpose AI technologies, are expected to revolutionise the application of AI in society and the economy. However, many scientists and politicians are calling for the establishment of a legal and ethical framework to avoid potentially detrimental impacts from the use of such technologies” (European Parliament 2023). In 2021, the European Commission proposed the AI Act to regulate this area (European Union 2021), but that regulation is still being debated (European Parliament 2023) and is expected to come into force in 2024. The EU Commission proposes in the AI Act that member states must appoint or establish at least one supervisory authority that will be responsible for ensuring that the “necessary procedures are followed” to ensure ethical and secure AI. According to European Parliament recommendations from May 2022, “AI has huge potential to boost capital and labour productivity, innovation, growth and job creation. However, its development could also pave the way for potential mass surveillance and other detrimental impacts on fundamental rights and values”.
Overall, image generative AI has several limitations that need to be addressed before it can be widely used in medical imaging and other applications. It is important to carefully evaluate the performance of these models and to develop methods for controlling and addressing their limitations.
In this article we have seen the possibilities that generative image AI can contribute to radiology and biomodels (some already possible and others future). We have also shown some of the current limitations. But all this leads us to a broader reflection at the present time. General generative AI in radiology is still under development, raising two questions for the future: how will it affect the management of imaging departments? And what will be the impact on professionals?
What Will Be the Main Impact in Healthcare System Management of Generative AI in Radiology?
The impact of generative AI in radiology is expected to be significant in the healthcare system business. Here are some potential effects:
- Improved Accuracy: Generative AI in radiology can help to improve the accuracy of diagnoses. By leveraging large datasets and advanced algorithms, generative AI can identify subtle patterns and anomalies in medical images that may be difficult for human radiologists to detect. This can lead to earlier and more accurate diagnoses, which can improve patient outcomes and reduce costs.
- Increased Efficiency: Imaging departments often face backlogs of images that need to be reviewed by imagers, which can lead to delays in diagnosis and treatment. Generative AI can help to alleviate this bottleneck by automatically triaging images, flagging urgent cases for immediate review, and routing less urgent cases to imagers for review at a later time. This can help to reduce wait times for patients and improve overall efficiency.
- Cost Savings: By improving accuracy and efficiency, generative AI in imaging can help to reduce healthcare costs. Earlier and more accurate diagnoses can lead to faster and more effective treatments, which can reduce the need for costly interventions such as surgeries or extended hospital stays. Additionally, by automating routine tasks such as image triage and annotation, generative AI can free up imagers to focus on more complex cases, which can improve overall productivity and reduce costs.
- Better Resource Allocation: Generative AI can help healthcare systems to better allocate resources by identifying urgent cases that require immediate attention and prioritising them accordingly. This can help to ensure that resources such as imaging equipment and staff time are used most efficiently.
- Data-Driven Decision-Making: Generative AI can help to provide healthcare managers with valuable insights into patient outcomes, resource utilisation, and other key performance indicators. This can help to inform data-driven decision-making and optimise healthcare system performance.
- New Opportunities for Innovation: As generative AI becomes more widely adopted in radiology, it is likely to open up new opportunities for innovation in the healthcare industry. For example, it may be possible to use generative AI to develop new imaging modalities or to identify new biomarkers for diseases. This could lead to the development of new diagnostic tools and therapies that could improve patient outcomes and reduce costs.
Overall, the impact of generative AI in radiology is expected to be significant, with potential benefits for patients, healthcare providers, and the healthcare industry as a whole. The speed and capacity of adoption and its impact will depend on the ability to integrate this new technology into healthcare systems and hospitals and its professionals, and this depends on the business models, regulation, ethical considerations and incentives. The speed of emergence and growth of this technology has meant that these questions have yet to be defined and we will see how they develop in the coming months and years. Probably, in a near future, we will see the expansion of proprietary Generative AI applications developed to solve specific complex tasks based on proprietary data.
How Will all This Affect the Future Imaging Job Situation? Training, Description, Content and Numbers
While generative AI in imaging has the potential to improve efficiency and accuracy, it is unlikely to completely replace the need for human professionals in the field. Rather, it is likely to transform the role of radiologists and other healthcare professionals involved in imaging.
Generative AI can help automate routine tasks such as image triage and annotation, freeing up radiologists to focus on more complex cases and to spend more time with patients. This can improve productivity and enable radiologists to provide more personalised care.
At the same time, generative AI may also create new job opportunities for healthcare professionals with expertise in data science and machine learning. These professionals may be needed to help develop and implement generative AI algorithms, as well as to analyse and interpret the results generated.
In summary, while the adoption of generative AI in radiology may change the role of imagers and other healthcare professionals involved in imaging, it is unlikely to completely replace the need for these professionals. Rather, it is likely to transform the nature of their work and create new opportunities for professionals with expertise in data science and machine learning. Thus, it is of most importance to introduce new skills and knowledge to the actual curricula of radiological and imaging specialties studies.
Conflict of Interest:
“All the images and part of the written content was created using a Generative AI”
References:
Adams LC, Truhn D, Busch F, Kader A, Niehues SM, Makowski MR & Bressem KK (2023). Leveraging GPT-4 for Post Hoc Transformation of Free-Text Radiology Reports into Structured Reporting: A Multilingual Feasibility Study. Radiology, 230725.
Antel R, Abbasgholizadeh-Rahimi S, Guadagno E, Harley JM & Poenaru D (2022) The use of artificial intelligence and virtual reality in doctor-patient risk communication: A scoping review. Patient Education and Counseling.
European Parliament (2023). Artificial Intelligence. European Parliamentary Research Service [EPRS]. Available from: https://www.europarl.europa.eu/RegData/etudes/BRIE/2023/745695/EPRS_BRI(2023)745695_EN.pdf
European Parliament (2023) Proposal for a Regulation on a European approach for Artificial Intelligence. Legislative Train Schedule European Parliament. Available from: https://www.europarl.europa.eu/legislative-train/theme-a-europe-fit-for-the-digital-age/file-regulation-on-artificial-intelligence
European Union (2021) Proposal for a REGULATION OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL LAYING DOWN HARMONISED RULES ON ARTIFICIAL INTELLIGENCE (ARTIFICIAL INTELLIGENCE ACT) AND AMENDING CERTAIN UNION LEGISLATIVE ACTS. EUR-Lex. Available from: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A52021PC0206
Freedman JD & Nappier IA (2023) GPT-4 to GPT-3.5:'Hold My Scalpel'--A Look at the Competency of OpenAI's GPT on the Plastic Surgery In-Service Training Exam. arXiv preprint arXiv:2304.01503.
Kung TH, Cheatham M, Medenilla A, Sillos C, De Leon L, Elepaño C et al. (2023) Performance of ChatGPT on USMLE: Potential for AI-assisted medical education using large language models. PLOS Digit Health 2(2): e0000198.
Laino ME, Cancian P, Politi LS, Della Porta MG, Saba L, Savevski V (2022) Generative Adversarial Networks in Brain Imaging: A Narrative Review. Journal of Imaging. 8(4):83.
Lee P, Goldberg C & Kohane I (2023) The AI Revolution in Medicine: GPT-4 and Beyond. 1st edition; Pearson (2023). ISBN-13: 9780138200138
Mulé S, Lawrance L, Belkouchi Y, Vilgrain V, Lewin M, Trillaud H, Hoeffel C, Laurent V, Ammari S, Morand E, Faucoz O, Tenenhaus A, Cotten A, Meder JF, Talbot H, Luciani A, Lassau N (2023) Generative adversarial networks (GAN)-based data augmentation of rare liver cancers: The SFR 2021 Artificial Intelligence Data Challenge. Diagnostic and Interventional Imaging. 104(1):43-48.
Nori H, King N, McKinney SM, Carignan D, & Horvitz E (2023) Capabilities of GPT-4 on Medical Challenge Problems. arXiv preprint arXiv:2303.13375.
The Economist (2023). The Economist of Corea: Samsung and ChatGPT. Available from: https://economist.co.kr/article/view/ecn202303300057?s=31
The Italian Data Protection Authority (2023) Intelligenza artificiale: Il Garante blocca ChatGPT. Raccolta illecita di dati personali. Assenza di sistemi per la verifica dell’età dei minori. Available from: https://www.garanteprivacy.it/web/guest/home/docweb/-/docweb-display/docweb/9870847




