Noninvasive evaluation of central venous pressure (CVP) is a component of the physical examination that can be very valuable in patient care, especially in the assessment of volume status. CVP estimates can be achieved by assessing the jugular venous pressure (JVP), peripheral venous collapse (PVC), and ultrasound visualisation of the inferior vena cava (IVC). Bedside evaluation of CVP dates back to the 1920s following Starling's cardiac haemodynamic experiments linking it to cardiac output.
However, the relative accuracy of these techniques compared to one another and their application by trainees of varying experience remains uncertain. A recent study compared the application and utility of the JVP, PVC, and handheld Mini Echo amongst trainees of varying experience including a medical student, internal medicine resident, and cardiology fellow. The authors also introduced and validated a new physical exam technique, the Anthem sign, to assess CVP.
Study Method
This study was conducted at St. Boniface Hospital's Echo Department in Winnipeg, Manitoba, with formal ethics approval from the University of Manitoba. A cohort of in- and out-patients presenting for their regularly scheduled echocardiograms provided consent for clinical evaluation of CVP using these non-invasive bedside techniques: the JVP, PVC techniques, and the handheld mini Echo. Patients were excluded if they had intravenous catheters in the right-sided veins and/or were not able to give informed consent.
JVP evaluation: CVP estimates are obtained by determining the height of the internal jugular venous waveforms relative to the sternal angle. CVPs are considered elevated when the height of the venous column is greater than three centimetres above the sternal angle. The right internal jugular vein was initially evaluated since it communicates with the right atrial in a relatively straight course. If the venous wave-forms of the right internal jugular vein were not well visualised, the left internal jugular vein was evaluated.
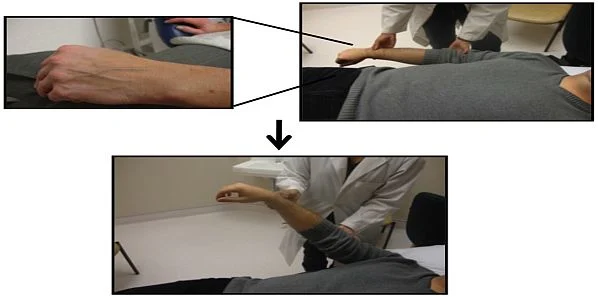
PVC techniques: In the supine position with a 30-degree elevation in the head of the bed, the patient's arms are rested on the side of the body and the dorsum of the hand is inspected for superficial veins. If the veins are not visible, this technique cannot be applied and if visible but collapsed already the CVP is likely low or normal. If the veins remain distended above the sternal angle, the CVP is likely elevated. As the observation point of PVC on the dorsum of the hand and the reference point at the sternal angle are quite far apart, the precise determination of the level of PVC is subject to error.
In an attempt to overcome such limitations, the investigators modified the classic PVC technique and introduced and validated a new physical exam method called the Anthem sign. In this position, the patient appears as an individual standing in attention for a national anthem. The new technique begins in a similar fashion as the classic PVC method. However, when the arm is ready to be passively elevated, it is simply placed directly over the sternum. In this approach, the PVC observation point on the dorsum of the hand and the reference point at the sternum are in close proximity and if the veins remain distended while rested on top of the sternum the CVP is thought to be elevated.
Bedside Mini-Echo: A handheld ultrasound device was used to assess the IVC to estimate CVPs as outlined by the American Society of Echo 2010 guidelines.
The investigators compared the application and utility of these techniques amongst three trainees of varying experience: a second year medical student with limited clinical experience, a second year medical resident with three years of clinical experience, and a second year cardiology fellow with six years of clinical experience. Forty-two patients were examined by both the medical student and resident independently to assess inter-observer agreement.
Prior to patient recruitment for the study, the medical student received focused training on the application of the JVP and PVC techniques by examining 44 patients over a period of one week, totalling an estimated teaching time of 10 hours. The internal medicine resident only received very brief instruction on the application of the physical exam techniques based on a patient assessment. Finally, the cardiology fellow did not require tutelage on the application of the bedside physical exam techniques. The Mini Echo was only utilised by the medical student following 10 hours of Echo training.
The examiners were blinded to the echo results, each other's assessments, and patient history; their CVP estimates were compared to the gold standard level 3 echo-cardiographer's estimates at the completion of the study.
Results
In total, 325 patients combined were examined: 217 by the medical student, 58 by the medical resident, 49 by the cardiology fellow, and 43 evaluated using Mini-Echo assessments. The average age was 65 (s.d.16) years with a mean BMI of 28 kg/m2 (s.d.6), and 52 percent were males.
When compared to the gold standard of CVP by a level 3 echocardiographer, the JVP was the most sensitive at 86 percent, improving with clinical experience (p<0.01). This rising trend in sensitivity with clinical experience was partly, but not completely, offset by a declining trend in specificity.
When applied by the examiner with the least clinical experience, the PVC techniques, with the Anthem sign in particular, had greater sensitivity than the JVP at 21 percent vs. 13 percent. Similar trends were observed in the evaluation of obese patients. After only brief echo training, the Mini-Echo assessments by the medical student were the most sensitive, at 100 percent.
When applied by the cardiology fellow, the Anthem sign had higher specificity than the JVP (85 percent vs. 57 percent, respectively). Amongst all three trainees, the classic PVC technique and Anthem sign had better specificity compared to the JVP, especially amongst obese patients.
In terms of inter-observer agreement, the patterns of sensitivities and specificities for bedside clinical exam techniques were similar in the 42 co-examined patients, as compared to the complete sub-group of patients examined by the medical student and resident.
Conclusion
JVP evaluation is the most sensitive physical examination technique in CVP assessments and its application improves with clinical experience. The PVC techniques along with the newly described Anthem sign may be of value for the early learner who still has not mastered the art of JVP assessment and in obese patients in whom JVP evaluation is problematic.
Mini-Echo estimates of CVPs are comparable to physical examination by trained clinicians and require less instruction. The use of Mini-Echo in medical training should be further evaluated and encouraged.
Image Credit: National Center for Biotechnology Information, US National Library of Medicine
However, the relative accuracy of these techniques compared to one another and their application by trainees of varying experience remains uncertain. A recent study compared the application and utility of the JVP, PVC, and handheld Mini Echo amongst trainees of varying experience including a medical student, internal medicine resident, and cardiology fellow. The authors also introduced and validated a new physical exam technique, the Anthem sign, to assess CVP.
Study Method
This study was conducted at St. Boniface Hospital's Echo Department in Winnipeg, Manitoba, with formal ethics approval from the University of Manitoba. A cohort of in- and out-patients presenting for their regularly scheduled echocardiograms provided consent for clinical evaluation of CVP using these non-invasive bedside techniques: the JVP, PVC techniques, and the handheld mini Echo. Patients were excluded if they had intravenous catheters in the right-sided veins and/or were not able to give informed consent.
JVP evaluation: CVP estimates are obtained by determining the height of the internal jugular venous waveforms relative to the sternal angle. CVPs are considered elevated when the height of the venous column is greater than three centimetres above the sternal angle. The right internal jugular vein was initially evaluated since it communicates with the right atrial in a relatively straight course. If the venous wave-forms of the right internal jugular vein were not well visualised, the left internal jugular vein was evaluated.
PVC techniques: In the supine position with a 30-degree elevation in the head of the bed, the patient's arms are rested on the side of the body and the dorsum of the hand is inspected for superficial veins. If the veins are not visible, this technique cannot be applied and if visible but collapsed already the CVP is likely low or normal. If the veins remain distended above the sternal angle, the CVP is likely elevated. As the observation point of PVC on the dorsum of the hand and the reference point at the sternal angle are quite far apart, the precise determination of the level of PVC is subject to error.
In an attempt to overcome such limitations, the investigators modified the classic PVC technique and introduced and validated a new physical exam method called the Anthem sign. In this position, the patient appears as an individual standing in attention for a national anthem. The new technique begins in a similar fashion as the classic PVC method. However, when the arm is ready to be passively elevated, it is simply placed directly over the sternum. In this approach, the PVC observation point on the dorsum of the hand and the reference point at the sternum are in close proximity and if the veins remain distended while rested on top of the sternum the CVP is thought to be elevated.
Bedside Mini-Echo: A handheld ultrasound device was used to assess the IVC to estimate CVPs as outlined by the American Society of Echo 2010 guidelines.
The investigators compared the application and utility of these techniques amongst three trainees of varying experience: a second year medical student with limited clinical experience, a second year medical resident with three years of clinical experience, and a second year cardiology fellow with six years of clinical experience. Forty-two patients were examined by both the medical student and resident independently to assess inter-observer agreement.
Prior to patient recruitment for the study, the medical student received focused training on the application of the JVP and PVC techniques by examining 44 patients over a period of one week, totalling an estimated teaching time of 10 hours. The internal medicine resident only received very brief instruction on the application of the physical exam techniques based on a patient assessment. Finally, the cardiology fellow did not require tutelage on the application of the bedside physical exam techniques. The Mini Echo was only utilised by the medical student following 10 hours of Echo training.
The examiners were blinded to the echo results, each other's assessments, and patient history; their CVP estimates were compared to the gold standard level 3 echo-cardiographer's estimates at the completion of the study.
Results
In total, 325 patients combined were examined: 217 by the medical student, 58 by the medical resident, 49 by the cardiology fellow, and 43 evaluated using Mini-Echo assessments. The average age was 65 (s.d.16) years with a mean BMI of 28 kg/m2 (s.d.6), and 52 percent were males.
When compared to the gold standard of CVP by a level 3 echocardiographer, the JVP was the most sensitive at 86 percent, improving with clinical experience (p<0.01). This rising trend in sensitivity with clinical experience was partly, but not completely, offset by a declining trend in specificity.
When applied by the examiner with the least clinical experience, the PVC techniques, with the Anthem sign in particular, had greater sensitivity than the JVP at 21 percent vs. 13 percent. Similar trends were observed in the evaluation of obese patients. After only brief echo training, the Mini-Echo assessments by the medical student were the most sensitive, at 100 percent.
When applied by the cardiology fellow, the Anthem sign had higher specificity than the JVP (85 percent vs. 57 percent, respectively). Amongst all three trainees, the classic PVC technique and Anthem sign had better specificity compared to the JVP, especially amongst obese patients.
In terms of inter-observer agreement, the patterns of sensitivities and specificities for bedside clinical exam techniques were similar in the 42 co-examined patients, as compared to the complete sub-group of patients examined by the medical student and resident.
Conclusion
JVP evaluation is the most sensitive physical examination technique in CVP assessments and its application improves with clinical experience. The PVC techniques along with the newly described Anthem sign may be of value for the early learner who still has not mastered the art of JVP assessment and in obese patients in whom JVP evaluation is problematic.
Mini-Echo estimates of CVPs are comparable to physical examination by trained clinicians and require less instruction. The use of Mini-Echo in medical training should be further evaluated and encouraged.
Image Credit: National Center for Biotechnology Information, US National Library of Medicine
References:
Rizkallah J, Jack M, Saeed M, Shafer L A, Vo M, Tam J (2014)
Non-Invasive Bedside Assessment of Central Venous Pressure: Scanning
into the Future. PLoS One. 2014; 9(10): e109215. PMCID: PMC4184858
Latest Articles
Cardiology, Ultrasound, CVP, atrial, physical examination
Noninvasive evaluation of central venous pressure (CVP) is a component of the physical examination that can be very valuable in patient care, especially in...