Concerns about ionising radiation during interventional cardiology have increased in recent years due to rapid growth in interventional procedure volumes and the high radiation doses associated with some procedures. Noncancer radiation risks to cardiologists and medical staff in terms of radiation-induced cataracts and skin injuries for patients appear to be clear potential consequences of interventional cardiology procedures, while a radiation-induced potential risk of developing cardiovascular effects remains less clear.
Medical exposure from X-rays and nuclear medicine is the largest man-made source of radiation exposure, representing a mean effective dose of 1.0–3.0 mSv per head per year. Although interventional cardiac procedures account for 12 percent of all radiological examinations, they are responsible for delivering the highest radiation dose (up to 50 percent of the total collective effective dose). Interventional cardiologists encounter much more radiation than most other medical staff due to their working position being close to the X-ray beam and the patient (the source of scatter radiation).
Radiation safety in the practice of interventional cardiology has been addressed by several professional bodies. In 2005, the American College of Cardiology (ACC) Foundation proposed interventional cardiology guidelines which emphasised that physicians are responsible for minimising the radiation injury hazard to their patients, professional staff, and themselves. In 2009, the American Heart Association (AHA) Science Advisory recommended the reference doses of common cardiology examinations, and in 2010 the ACC committee also expressed the need for appropriate and optimal use of radiation techniques in cardiology.
The current study provides an overview of the radiation-induced noncancer risks during interventional cardiology procedures, with a focus on the radiation risks to interventional cardiologists and patients, as well as strategies commonly undertaken to reduce radiation exposure.
Radiation-Induced Effects and Risks to Medical Staff
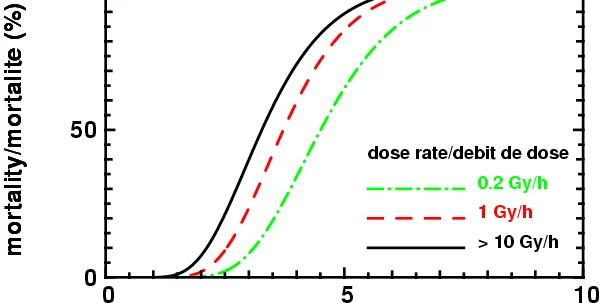
There are two main biological effects of ionising radiation: stochastic effects, which include carcinogenic and genetic effects and deterministic effects (also called tissue reactions), which refer to an immediate and very predictable change to the tissue. Radiation-induced cancer and genetic effects are stochastic in nature and this has been well addressed in the literature. Deterministic effects occur when the dose exceeds a specific threshold. The severity of deterministic effects commonly increases with dose, as more cells are killed or damaged. Common examples of deterministic effects related to interventional cardiology are skin and hair changes, cataracts, and cardiovascular disease.
- Radiation-Induced Cataracts
The National Council on Radiation Protection (NCRP) and the International Commission on Radiological Protection (ICRP) proposed guidelines on the view that cataractogenesis is a deterministic effect and requires a threshold radiation dose (currently 2 Gy). However, radiation-induced cataracts are reported in populations exposed to much lower doses than the current standards, and this strongly suggests a stochastic hypothesis.
Ionising radiation exposure has been linked to vision-impairing cataracts in atomic bomb survivors in a recent study, although further research is needed to focus on interventional cardiologists regarding radiation exposure and the development of cataracts.
- Radiation-Related Cardiovascular Diseases
Several studies have demonstrated the effects of ionising radiation on hematologic parameters and immunologic function; however, the question of whether radiation affects other physiologic phenomena, including arterial blood pressure, is still under debate despite continuous research efforts. Increased mortality risk was reported for heart disease, stroke, and respiratory diseases in the Life Span Study of atomic bomb survivors, with an excess relative risk for death from heart disease of 0.14 per sievert. Dose above 0.5 Gy was found to be associated with an elevated risk of both stroke and heart disease.
Epidemiological data on low dose radiation-induced damage to cardiovascular system are scare and conflicting: an increased cardiovascular disease risk was reported from studies of early radiologists in the USA but not from radiologists in the UK. More epidemiological studies are needed to help clarify the possible mechanisms between radiation exposure and its effect on the microcardiovascular damage.
Radiation-Induced Risks to Patients
Interventional cardiology procedures such as coronary angiography, percutaneous transluminal coronary angioplasty (PTCA), radiofrequency ablation, electrophysiological study, and left ventriculography contribute a significant proportion of radiation dose to patients due to the long fluoroscopy times and high-quality images required.
Patient radiation dose varies widely not only among different interventional cardiology procedures but also among published studies. Discrepancies of the available results in the literature are patient-, procedure-, cardiologist-, and fluoroscopic equipment-related. Interventional cardiology procedures can expose patients to high radiation doses, so efforts to minimise patient exposure should always be undertaken.
- Radiation-Induced Skin Injury
The skin is the organ most at risk during complex interventional procedures. Skin changes such as erythema, ulcers, telangiectasia, and dermal atrophy are well-known deterministic effects of ionising radiation. An early response (early transient ischemia) is noticed a few hours after doses greater than 2 Gy, when the exposed area is relatively large. An actual skin dose in the 5–10 Gy range will always produce a noticeable injury with doses above 15 Gy leading to tissue being destroyed to a depth of a few centimetres and dermal necrosis. To minimise this risk, evaluation and assessment of maximum skin dose in interventional cardiology procedures are of paramount importance and should be recommended in daily practice, although it is very difficult to undertake.
Strategies to Reduce Radiation Risks to Staff and Patients
Several aspects of radiation safety in interventional cardiology have been proposed with effective dose reduction outcomes having been achieved. These include strategies of dose monitoring during the procedure (i.e., special dosimeters to monitor doses to the skin, hands, feet, and the lens of eyes); wearing protective devices (e.g., lead apron, thyroid shield, leaded glass, etc.); applying dose-reduction techniques (i.e., increasing patient’s distance from the radiation source); and implementing training and education programmes.
Summary and Conclusion
There is increasing concern about the potential deleterious effects from radiation arising from interventional cardiology for two reasons: first, cardiac procedure volumes have grown tremendously. Second, the radiation doses received by interventional cardiologists and patients can vary by more than an order of magnitude for the same type of procedure. Increased workload, the complexity of interventional procedures, and acute patient conditions contribute significantly to the amount of radiation exposure to both patients and medical staff.
Noncancer risks of radiation in interventional cardiology that have been discussed in different scenarios emphasise the importance of reducing radiation dose to patients and medical staff. This can be achieved through implementing necessary strategies such as continual improvements in protocols and equipment, the implementation of guidelines proposed by professional bodies into daily practice, and attending training programmes to ensure best practices. Epidemiological studies involving a large cohort of individuals exposed to ionising radiation will help determine the true effects of radiation exposure from interventional cardiology.
Reference:
Zhonghua Sun, Aini AbAziz, and Ahmad Khairuddin Md Yusof. BioMed Research International Volume 2013 (2013), Article ID 976962, 11 pages
http://dx.doi.org/10.1155/2013/976962
Image credit: Wikipedia
Latest Articles
Cardiology, Radiology, Angiography, Angioplasty, ionising radiation
Concerns about ionising radiation during interventional cardiology have increased in recent years due to rapid growth in interventional procedure volumes a...