Stable coronary artery disease (CAD) patients who are neither experiencing a heart attack nor an abnormal stress test, may not be receiving additional benefits from angioplasty for the treatment of their narrowed arteries when compared to drug therapy alone. This was revealed in a recent Stony Brook University School of Medicine cardiologists-led survey of more than 4,000 patients with myocardial ischemia, or inadequate circulation, and published in the online first edition of JAMA Internal Medicine.
David L. Brown, MD, and Kathleen Stergiopoulos, MD, PhD, Professors in the Department of Medicine, Division of Cardiovascular Medicine at Stony Brook University School of Medicine co-authored the report entitled "Percutaneous Coronary Intervention Outcomes in Patients With Stable Obstructive Coronary Artery Disease and Myocardial Ischemia: A Collaborative Meta-analysis of Contemporary Randomized Clinical Trials,". They conducted the research by working with international colleagues in their aim to combined data from clinical trials performed between 1970 and 2012 of patients who had received either percutaneous coronary intervention (PCI), or angioplasty, plus drug therapy, or drug therapy alone as treatment for their CAD.
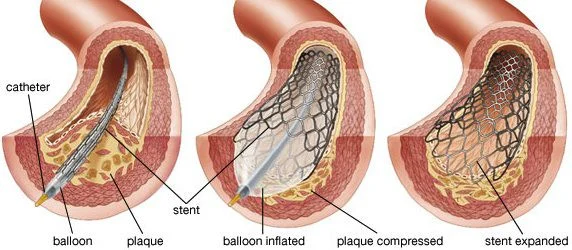
The analysis of the individual clinical studies reported outcomes of death and nonfatal myocardial infarction, and in order to reflect contemporary interventional and medical practice, inclusion criteria required stent implantation in at least 50 percent of the PCI procedures and statin medications to lower cholesterol in at least 50 percent of patients, in both the PCI and drug therapy alone groups.
As a consequence, there were five clinical trials yielding over 4,000 patients with myocardial ischemia diagnosed by exercise stress testing, nuclear or echocardiocraphic stress imaging, or fractional flow reserve.
Outcome data from up to five years post PCI or drug treatment alone was reviewed by the researchers, who analysed all-cause death, unplanned revascularisation, angina and non-fatal myocardial infarction in the patients.
Results in all-cause death rates between the two groups was not significantly different: 6.5% for patients receiving PCI and drug therapy versus 7.3% for those receiving drug therapy alone. Furthermore, the rates of non-fatal myocardial infarction (9.2% with PCI vs. 7.6% drug therapy) and recurrent or persistent angina (20.3% vs. 23.3%) showed very small differences. The rate of unplanned revascularisation was a little different without being statistically significant (18.3% vs. 28.4%).
Dr. Brown stated that in case these findings were confirmed in further trials, a large number of the 10 million+ annual stress tests and subsequent revascularisations may be unnecessary. He went on to caution that supplementary studies beyond data analyses of clinical trials were vital in order to absolutely determine if common applications of PCI in stable CAD patients needed to be re-assessed and if so, under what circumstances and in which patient populations.
Source: Science Daily
Photo credit: Encyclopeadia Britannica
7 December 2013
Latest Articles
Research, PCI, Stent, cardiac arrest, Angioplasty
Stable coronary artery disease (CAD) patients who are neither experiencing a heart attack nor an abnormal stress test, may not be receiving additional bene...