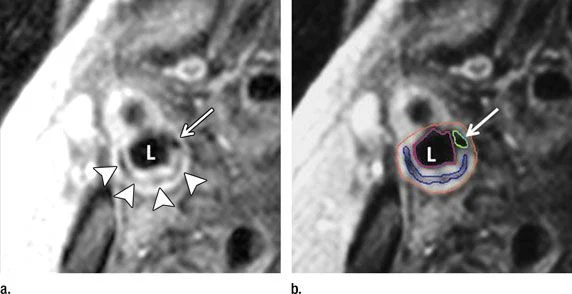
Figure 1. Transverse gadolinium-enhanced T1-weighted MR images obtained superior to the carotid artery bifurcation in a 72-year-old man. L = ICA lumen. (a) Low-signal-intensity calcium (arrow) and lipid core (arrowheads) can be seen. (b) Note contouring of the ICA. The outer adventitial wall (red), lipid core (blue), calcification (green), and vessel lumen (purple) are visible.
Findings of a new study published online in the journal Radiology state that noninvasive imaging of carotid artery plaque with MRI in people without a prior history of cardiovascular disease can conclusively indicate the likelihood of future cardiovascular events such as strokes and heart attacks.
It is a known fact that some arterial plaque is more dangerous because of its vulnerability to rupture, and MRI’s ability to distinguish features of vulnerable plaque, such as a lipid core with a thin fibrous cap, makes it a potentially valuable tool for identifying patients at risk for subsequent cardiovascular events.
In order to study the predictive value of MRI plaque imaging researchers conducted carotid artery ultrasound and MRI on almost 950 asymptomatic patients from the Multi-Ethnic Study of Atherosclerosis (MESA). Carotid arteries, the large vessels located on each side of the neck, carry oxygenated blood to the front part of the brain. They are highly accessible for imaging, and their condition has the tendency to mirror that of the coronary arteries, which supply the heart with oxygenated blood.
Using ultrasound to assess carotid wall thickness and MRI to define carotid plaque composition and the remodeling index, a measure of changes in vessel size, researchers compared imaging results with cardiovascular events, including heart attacks, stroke and death, for an average of 5.5 years after examination.
David A. Bluemke, MD, PhD, from the National Institutes of Health Clinical Center in Bethesda, Md, outlined how the team studied asymptomatic individuals with a low risk of cardiovascular events at baseline and used noninvasive imaging to predict the risk of an event downstream. Bluemke pointed out that this prospective study was the first population-based research conducted with the aim of establishing whether vulnerable plaque features by MRI added to the risk of a cardiovascular event beyond the traditional risk factors.
The study revealed that 59 patients suffered cardiovascular events, abnormal thickening of the carotid artery wall and the presence of a lipid core and calcium in the internal carotid artery on MRI were significant predictors of subsequent events. In almost half of the patients who had an event, a lipid core was present, whereas this was only the case for 17.8 percent of those who did not have an event.
Use of MRI provided a better outcome for the reclassification of baseline cardiovascular risk in the study group. When risk stratification was based on both the carotid remodeling index and lipid core, in comparison with the use of traditional risk factors roughly 16 percent more patients with events and 7 percent without events were correctly reclassified.
According to Dr Bluemke the results bolster the use of MRI as a surrogate marker of efficacy in therapeutic studies and suggest a role in assessing which patients might require more aggressive treatments. He went on to say that with the improvement of risk factor prediction, it will be possible to screen more intelligently and apply more intensive treatments in those individuals faced with a higher risk of cardiovascular events.
In conclusion Dr Bluemke noted that sequences for plaque composition could be readily added to existing carotid MRI angiography protocols for clinical purposes, as carotid MRI results were more reproducible than those of ultrasound.
While availability and cost effectiveness could limit the use of MRI, ultrasound and computed tomography (CT) presented viable alternatives for screening, especially with improvements in CT dose reduction.
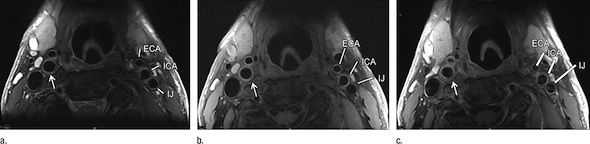
Figure 2. Transverse (a) T2-weighted, (b) unenhanced T1-weighted, and (c) gadolinium-enhanced T1-weighted MR images in an 82-year-old man. Pulse sequence parameters are described in Table 1. The left ICA wall shows no plaque or significant wall thickening. The right ICA shows plaque with a lipid core (arrow).ECA = external carotid artery, IJ = internal jugular vein.
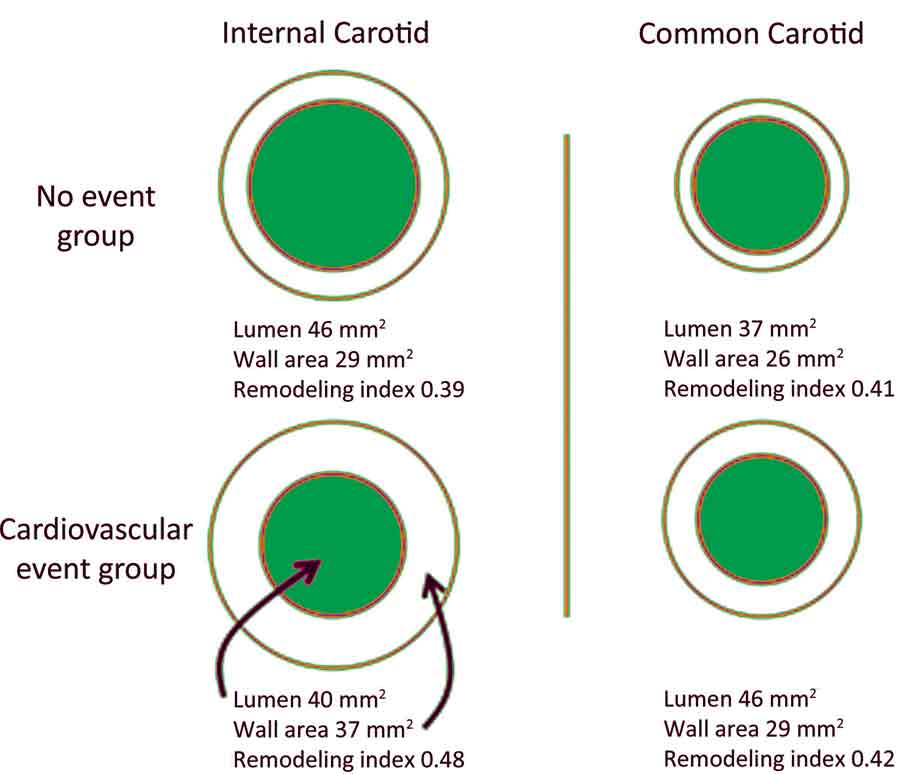
Figure 3. Diagram shows representative changes in carotid wall area, lumen area, and remodelling index for the ICA and CCA. Representative values of lumen and wall areas are taken from Table 1. The normal remodeling index tends to be approximately 0.4 independent of vessel size. The remodelling index increases with relatively increased atherosclerotic burden. Diagrams are not to scale.
Source: RSNA
4 March 2014
Latest Articles
CT, Stroke, MRI, Ultrasound, heart attack, plaques, CT angiography, carotid artery
Figure 1. Transverse gadolinium-enhanced T1-weighted MR images obtained superior to the carotid artery bifurcation in a 72-year-old man. L = ICA lumen. (a)...