A study comparing an invasive strategy with optimal medical therapy alone in older adults following a non-ST-elevation myocardial infarction (NSTEMI) found no impact on the combined risk of cardiovascular death or myocardial infarction (MI), despite reductions in non-fatal MIs and subsequent revascularisation procedures. This finding was presented at ESC Congress 2024, based on the SENIOR-RITA trial, published in the New England Journal of Medicine.
Current guidelines recommend an invasive strategy over medication alone for higher-risk patients post-NSTEMI. However, older patients are less likely to receive such care, possibly due to fears of procedural complications or lack of clear evidence, as older adults are underrepresented in clinical trials. This leads to non-standardised care for NSTEMI in this age group.
In this trial, researchers hypothesised that an invasive strategy plus optimal medical therapy would outperform optimal medical therapy alone in reducing cardiovascular death or non-fatal MI in patients aged ≥75 years with NSTEMI. There was no reduction in the combined risk of cardiovascular death or non-fatal MI, but there was a decrease in recurrent non-fatal MIs and the need for subsequent revascularisation.
In the trial, 1,518 patients aged ≥75 years with type 1 NSTEMI were randomly assigned to either a conservative strategy with optimal medical therapy or an invasive strategy involving coronary angiography and possible revascularisation. All patients received guideline-recommended secondary prevention medications, including antiplatelets, statins, ACE inhibitors, and beta-blockers. Frailty, cognition, and comorbidities were assessed at baseline and follow-up, with the primary endpoint being time to cardiovascular death or non-fatal MI. Secondary endpoints included all-cause death, revascularisation, and bleeding complications.
Participants had an average age of 82.4 years, with 72% aged 80 or older. Nearly half were female, 80% were classified as prefrail or frail, over 60% had cognitive impairment, and most had a comorbidity index of ≥5. In the invasive group, 90% underwent angiography, and 50% had revascularisation during hospitalisation.
After a median follow-up of 4.1 years, the primary endpoint occurred in 25.6% of the invasive group and 26.3% of the conservative group. No significant differences were found in cardiovascular death (15.8% invasive vs. 14.2% conservative). However, non-fatal MI rates were lower in the invasive group (11.7% vs. 15.0%), and the need for subsequent revascularisation was reduced (3.9% vs. 13.7%). Other secondary outcomes, including all-cause death, combined MIs, stroke, heart failure hospitalisation, or bleeding complications, showed no significant differences. Procedural complications occurred in less than 1% of cases.
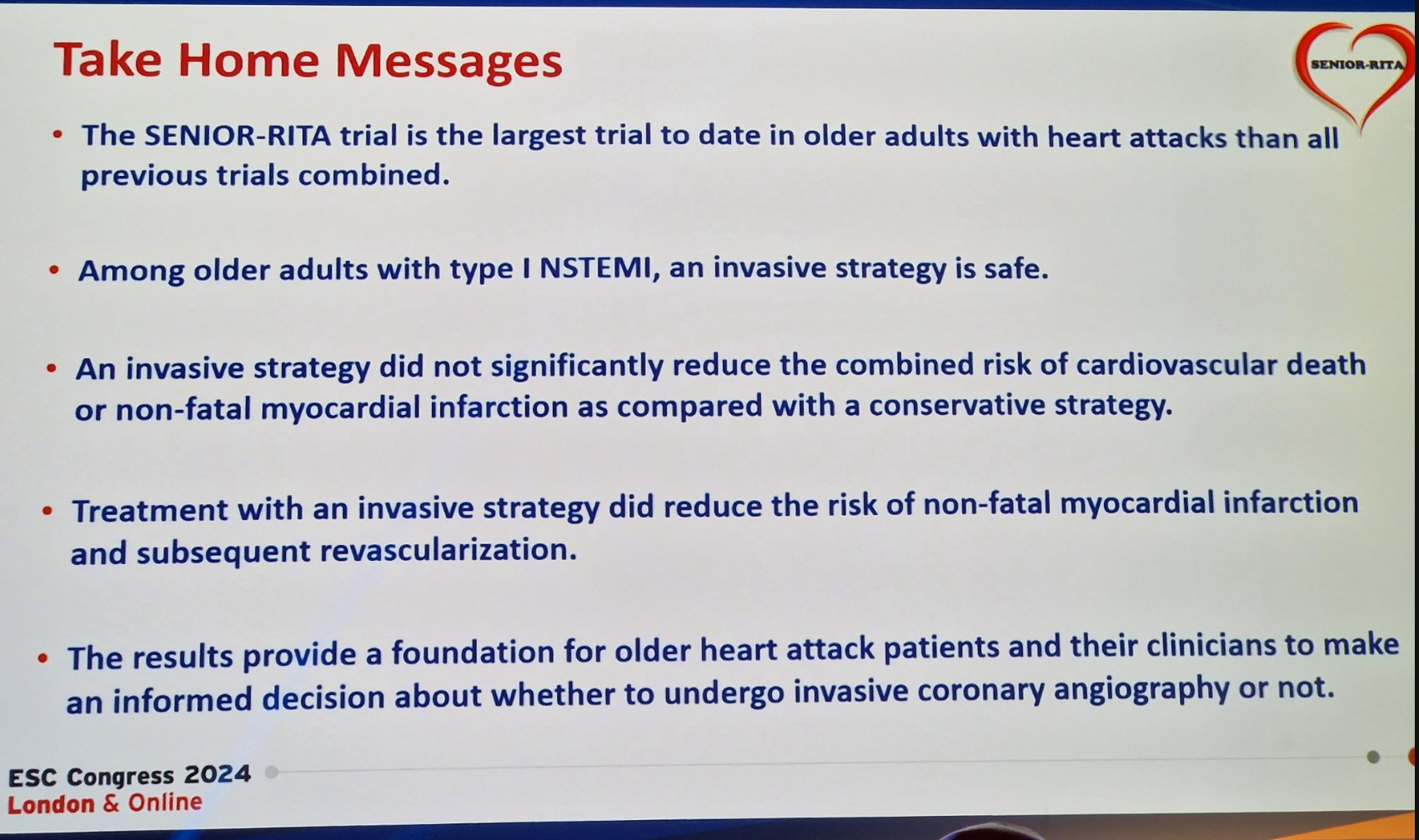
Overall, the study shows that while an invasive strategy did not reduce the primary endpoint, it showed some benefits and appeared safe in older patients. These findings underscore that age should not limit access to individualised care, including angiography and percutaneous coronary intervention.
Source, Slide and Image Credit: ESC Congress 2024