A groundbreaking study presented at the Society of Interventional Radiology Annual Scientific Meeting unveils the potential of a minimally invasive treatment for prostate cancer using MRI-guided transurethral ultrasound ablation (TULSA). This innovative approach offers an effective alternative to traditional treatments like surgery or radiation, which often come with significant side effects such as urinary incontinence and erectile dysfunction. The research, led by Dr Steven S. Raman, a professor of radiology, urology, and surgery at the David Geffen School of Medicine at UCLA, marks a significant advancement in prostate cancer care.
The Need for Alternative Prostate Cancer Treatments
Prostate cancer is the most prevalent form of cancer in men, affecting one in eight men during their lifetimes. The high incidence rate underscores the importance of developing alternative treatments that can effectively manage the disease while minimising adverse effects on patients' quality of life. Dr Raman describes the success of TULSA as a revolutionary development in whole-gland treatment for prostate cancer, with the potential to change the standard of care for thousands of men worldwide. Dr Raman emphasised the critical role of interventional radiologists (IRs) in prostate cancer care, highlighting their expertise in imaging and image-guided procedures as essential components of the prostate cancer treatment team. He noted that IRs have already played significant roles in the detection and management of other cancer types, such as lung, kidney, and liver cancers, and their involvement in prostate cancer care is equally important.
The TULSA Procedure: Precision and Flexibility
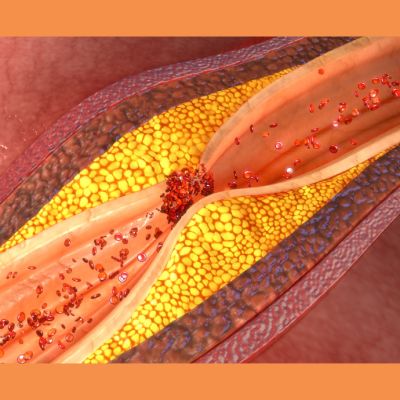
The TULSA procedure involves inserting a small catheter-like device through the urethra into the prostate gland. Utilizing MRI technology, precise positioning of therapeutic ultrasound elements is guided into the prostate, allowing for targeted treatment of cancerous tissues. MR thermometry is employed to monitor tissue temperatures, ensuring that the prostate tissue is heated to more than 55 degrees Celsius while protecting sensitive surrounding nerves. This precision targeting and monitoring enable the destruction of cancer cells while minimising damage to healthy tissues, achieving what Dr Raman refers to as the "ultimate trifecta" in prostate cancer treatment: full local cancer control, preservation of urinary continence, and maintenance of erectile function. One of the notable advantages of the TULSA procedure is its flexibility in treatment settings. The procedure can be performed in either outpatient or in-patient facilities under general or spinal anaesthesia, typically taking two to three hours to complete. This versatility allows for personalised treatment plans tailored to individual patient needs and preferences, enhancing overall treatment outcomes and patient satisfaction.
Multicentre Study Validates TULSA's Efficacy and Safety
The multicentre study involved 115 men recruited from 13 sites across five countries, providing a comprehensive evaluation of TULSA's efficacy and safety in diverse patient populations. Some participants required follow-up conventional treatments due to residual or new tumours, allowing researchers to identify early predictors of TULSA failure. Factors such as calcifications between the urethra and target prostate cancer and prostate swelling were identified as potential areas for improvement in procedure monitoring and management.
TULSA's Potential to Revolutionise Prostate Cancer Care
The study's findings highlight the effectiveness of TULSA in reducing cancer presence, prostate size, and prostate-specific antigen (PSA) levels, which are crucial markers for cancer progression. After undergoing the TULSA procedure, 76% of participants showed undetectable cancer on follow-up biopsies at one year. Additionally, there was a remarkable 92% reduction in median prostate volume within one year and a significant decrease in PSA levels from 6.3 ng/ml to 0.63 ng/ml at five years post-procedure. Comparative analysis with other treatment modalities such as surgery, radiation, and thermal therapy (US-guided HIFU or cryotherapy) revealed that TULSA offers a more favourable side-effect profile. By the five-year mark, 92% of patients regained continence, and 87% preserved erectile function, demonstrating the procedure's superior outcomes in terms of maintaining patients' quality of life.
The study's findings provide compelling evidence for the effectiveness and safety of MRI-guided transurethral ultrasound ablation (TULSA) as a minimally invasive treatment option for prostate cancer. With its ability to achieve excellent cancer control while preserving urinary continence and erectile function, TULSA has the potential to revolutionise prostate cancer care and become a new standard of treatment for men diagnosed with this prevalent and life-altering disease. Further research and validation are needed to confirm these promising results and expand access to this innovative treatment option for prostate cancer patients worldwide.
Source: Society of Interventional Radiology Annual Scientific Meeting
Image Credit: iStock