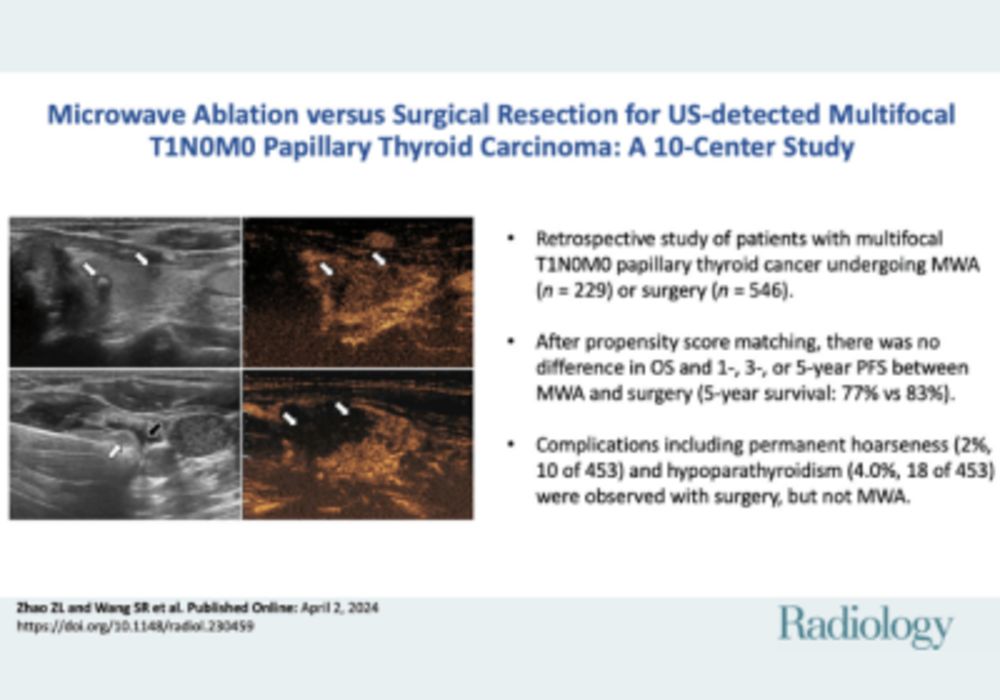
Papillary thyroid cancer (PTC) is the most common type of differentiated thyroid cancer, with multifocal occurrence ranging from 23.5% to 60%. While the 2015 American Thyroid Association guidelines don't classify multifocal PTC as high-risk, it's often treated as such, primarily through surgical resection (SR). Some studies even recommend total thyroidectomy due to the high multifocality rate. Despite this, the prognosis for multifocal PTC post-SR remains favourable, with 10-year recurrence-free survival rates between 83.2% and 87.3%. However, SR has drawbacks, including scarring, lifelong hormone replacement, and potential complications like hypoparathyroidism and hoarseness. A recent study published in Radiology aims to compare the progression-free survival (PFS) rates and complication rates between SR and MWA in cases of preoperative US-detected T1N0M0 multifocal PTC at overall, 1-, 3-, and 5-year intervals.
Microwave Ablation in Treating PTC: Efficacy, Safety, and Metastasis Concerns
Microwave ablation (MWA) has become popular for treating single-focus PTC due to its minimally invasive nature, efficacy, and safety. Treatment guidelines from Italy, Korea, and China endorse thermal ablation for unifocal PTC. For multifocal PTC, MWA and radiofrequency ablation are emerging as minimally invasive options, but comprehensive evidence on their efficacy and safety is lacking due to limited studies and sample sizes. Concerns exist about MWA's lack of routine prophylactic lymph node (LN) ablation, potentially leading to higher LN metastasis rates compared to SR, which commonly involves LN resection.
Retrospective Study from 10 Chinese Hospitals
This retrospective multicentre study involved 10 hospitals in China examined patients with multifocal papillary thyroid cancer (PTC) who underwent either microwave ablation (MWA) or surgical resection (SR) from May 2015 to December 2021. The study was approved by all participating hospitals' ethics committees, and the need for written informed consent was waived due to its retrospective nature. Inclusion criteria for the study were:
- Confirmed multifocal PTC with a maximum diameter of 2 cm via fine-needle aspiration or core-needle biopsy.-
- No evidence of metastasis on preoperative ultrasound (US) or chest CT (preoperative T1N0M0).
- Ineligibility for or refusal to undergo surgery in the MWA group (due to inability to tolerate general anaesthesia or tracheal intubation).
- No prior thyroid surgery.
- Minimum follow-up of 12 months.
Exclusion criteria included:
- Severe coagulation disorder or organ failure.
- Residence in a palliative care setting due to another malignant disease or expected survival of less than 2 years.
- Incomplete follow-up data.
After propensity score matching (PSM), 682 patients were enrolled: 229 in the MWA group and 453 in the SR group. From an initial pool of 4937 PTC patients, 775 met the inclusion criteria after excluding those with unifocal PTC, lymph node (LN) metastasis, lesions larger than 2 cm, less than 12 months of follow-up, and incomplete data. Before PSM, the median age of the MWA group was 44 years with 179 females, and they had 561 nodules. The SR group had a median age of 45 years with 442 females and 1482 nodules. After PSM, all 229 patients were in the MWA group, and 453 were in the SR group. The median follow-up was 20 months for MWA and 26 months for SR. Postoperative pathologic findings revealed that 64.5% of SR patients were in the SR-T1N0 subgroup, and 35.5% were in the SR-T1N1 subgroup. The study compared the findings of the PSM MWA group with those SR subgroups.
Survival and Complications for Thyroid Cancer patients
Thyroidectomy, the standard treatment for papillary thyroid cancer (PTC), often leads to lifelong hormone replacement and risks like permanent hoarseness (1.2%-3.6%) and hypoparathyroidism (1.4%-5.1%). In contrast, microwave ablation (MWA) has shown improved quality of life and fewer complications. A study comparing MWA and surgical resection (SR) for progression-free survival and complications found no significant difference in 1-, 3-, and 5-year survival rates (5-year rate: P = .36). However, MWA resulted in reduced transient hoarseness (P = .02) and permanent hypoparathyroidism (P = .005), as well as shorter incisions and hospital stays. The indolent nature of early-stage PTC leads to low tumour progression rates post-treatment. The MWA group in this study had a 4.8% tumour progression rate, consistent with prior research on multifocal (5.4%-6.4%) and unifocal (1.1%-4.0%) PTC. The SR group's tumour progression rates (3.5%-4.3%) also aligned with historical data (2.2%-6%). Despite slightly lower 3- and 5-year progression-free survival rates in the MWA group, differences were not significant.
Microwave Ablation shows lower rates of lymph node metastasis
Lymph node (LN) metastasis is common in PTC. Even though all patients were classified as T1N0M0 preoperatively, post-treatment LN metastasis rates were 35.5% after SR and 48.0% in previous meta-analyses, suggesting undetected micrometastases. MWA's LN metastasis rate during follow-up was lower (0.4%) than SR (1.3%), indicating that skipping prophylactic LN ablation during MWA doesn't increase LN metastasis rates compared to routine LN removal during SR. Major complications included hoarseness and permanent hypoparathyroidism, with rates consistent with prior studies. MWA had lower rates of transient hoarseness (3.1%) and permanent hypoparathyroidism (0%) compared to SR.
Study limitations include its retrospective nature, potential selection bias, lack of data on PTC subtypes in the MWA group, and relatively short follow-up time. Longer-term, prospective studies are needed to confirm these findings. For preoperative US-detected T1N0M0 multifocal PTC, MWA and SR showed similar progression-free survival rates, but MWA had fewer complications. MWA appears promising for treating multifocal PTC, but further research is needed for validation.
Source & Image Credit: RSNA Radiology