On 24 November, leading experts including Jorge Juan Fernández (EIT Health), John Halamka (Mayo Clinic) and medical futurist Bertalan Meskó discussed the opportunities and challenges of AI in healthcare.
You might also like:Let’s Talk About High-Value Care
The session Implementing AI in Healthcare: Success Beyond the Buzzword opened this year’s EIT Health Summit Series. The main conclusion that all participants agreed on was that AI was not the future but already a reality that stakeholders needed to embrace, and those not using AI would be replaced by those who used it.
After a brief introduction by Alexander von Gabain, Chairman of the Supervisory Board at EIT Health, Jan-Philipp Beck, CEO of EIT Health, and national EIT Health Managing Directors from France, Spain and Benelux, Dr Halamka presented the Mayo Clinic’s ‘Cure, Connect and Transform’ 2030 Plan.
AI by 2030
This plan is based on recognising that the digital future in healthcare is an imperative, and that business models must change because of the evolution in technology, policy and culture, especially in light of the COVID-19 pandemic.
Mayo’s digital transformation starts with data, said Dr Halamka. Since 154 years ago, when the clinic launched patient records, there are many longitudinal data coming from various sources and in various formats that need to be digitised, because the data of the past are used to inform the care of the future.
Challenges here are: privacy protection, compliance with GDPR and HIPPA regulations, cultural expectation that the data are being used in positive ways. Due to this, de-identified aggregated data are an imperative to protect privacy.
De-identification is extremely difficult. Mayo uses natural language processing and machine learning, and once the data have low probability of re-identification, they are put out to Google Cloud in an encrypted container with controlled access. Third parties can use them for their own R&D, but the data never leave Mayo’s control.
These de-identified data are used to create products and services through the so-called AI Factory, where Mayo’s AI tools are integrated. The AI Factory can be used by Mayo staff to explore new ideas, e.g. in radiation oncology, diagnostics of neuromuscular diseases, etc. Thanks to this, each department at Mayo starts to think in this ‘platform’ approach. It integrates the data about patient with EHRs, providers, payors, etc. through algorithms that generate value for Mayo, creating a completely new business model.
You might also like:New Era in High Value Care in Europe
For 2020-2030, digital therapeutics and virtual care are areas of focus for Mayo Clinic. COVID-19 has highlighted the importance of virtual care, which spans from simple actions like diagnostics by an AI chatbot or virtual visits, to highly complex care that traditionally required observation and treatment in a controlled hospital environment. In 2020, Mayo has developed an acute-care-at-home product, treating about 50 patients with serious and complex disease in their homes. The AI-driven system comprises monitors in patients’ homes and dashboards at the hospital’s command centre enabling specialists following the patient to ensure the right orders, interventions and care plans. This means same outcomes at a lower cost, Dr Halamka noted. By 2030, Mayo will see significant expansion in the amount of acute care delivered at a distance in non-traditional settings. For this, the next generation of professionals is being trained, and partnerships are formed for equipment delivery, supplies and local staffing. As such, Mayo aims to act as a care traffic controller with local paramedics and nurses working with the patient.
Another emerging area for Mayo’s AI utilisation is new kinds of telemetry, with many new devices coming to the market. There has been an explosion of new types of data, but signal needs to be separated from noise and data need to be turned in to action.
After Dr Halamka’s talk, the audience was invited to choose between a human doctor and an AI doctor in a poll, and about 80% still preferred to interact with a human doctor.
Extraordinary Challenges and Potential of AI
Dr Meskó opened his talk urging everyone to acknowledge that AI was not the future, but already a reality. He compared the situation with AI in healthcare with that in chess. After the Deep Blue algorithm famously defeated Garry Kasparov in 1997, many said chess was dead. However, its popularity has been growing ever since, and today chess is impossible without AI assistance to learn and understand new strategies.
Same is true for healthcare – for medical professionals, policymakers and patients alike. Their decisions are today supported by AI.
The potential was extraordinary, argued Dr Meskó citing progress in areas such as clinical trials or predictive diagnostics based on analysis of massive amounts of data. Patients as well are empowered to monitor their own health with the help of AI through, for example, wearables, DNA tests, or microbiome sequence analysis.
At the same time, challenges for AI in healthcare are also extraordinary and include privacy issues, lack of properly skilled workforce, bias in AI or the necessity to involve patients at the highest level of decision-making in algorithm design.
According to Dr Meskó, AI will not end the era of art in medicine, it will start it as soon as we understand how AI operates; AI will not replace physicians, but those physicians who use AI will replace those who do not. Therefore, it is a must-have.
Future of AI
The panel discussion that followed included three blocks: the potential of AI; risk and challenges; and recommendations for a CEO.
Asked about what will happen with AI in the next few years, Dr Halamka pointed out the growing need for care at a distance, which means more algorithms, more chatbots, more AI-enabled workflow. “There is no question that algorithms will explode in the next few years,” he noted. Dr Meskó shared this opinion commenting that it was obvious AI did certain tasks better than physicians, and that patients might actually be the driving force behind wider AI adoption in healthcare. He remarked, however, that AI would not be able to provide empathy in a way medical professionals could, or control the whole process of healthcare. Dr Halamka explained that data would always need curation and clean-up, “so we won’t see raw data used for AI algorithm development”, and that we needed “algorithms that augment human behaviour and not replace it”.
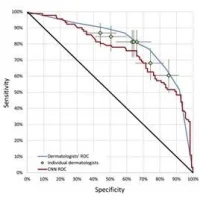
Prompted by another poll, the audience (64%) and the panellists agreed that there would not be many diagnostic processes that were not fully supported by AI in the next five to ten years.
Answering a question about who should be in control of a patient’s health data, over half of the respondents believed it should be individuals themselves; national governments and hospitals were voted by about 18% of respondents each.
Concluding the discussion, the speakers gave their recommendations to a CEO of a pharma/medtech company. According to Dr Halamka, “doctors will always need to be human empathetic people providing much more than just probabilistic and statistical analysis”. However, pharma, providers and payors should recognise that healthcare in the next five years will be a data business, so their future is in the curation of large data and the algorithms based on that data.
Dr Meskó stressed that patients were the biggest new player in the healthcare field, hence any CEO or decision-maker should embrace the concept of patient design. “Nobody should think that they are able to create services, technologies, medications, protocols, or treatments for patients without involving those patients at the highest level,” he said.
You can watch the full recording of the AI session here.