Colorectal cancer (CRC) is a prevalent and increasingly diagnosed malignancy worldwide, presenting significant health risks. Despite advancements in treatments like surgery, chemotherapy, and radiotherapy, CRC mortality rates remain high, especially in cases with distant metastases or recurrence after surgery. The TNM staging system, which evaluates tumour depth, lymph node involvement, and distant metastasis, is commonly used to assess prognosis but has limitations.
Recent studies have highlighted the role of body composition analysis using CT scans in predicting outcomes for CRC patients post-surgery. Unlike traditional indicators like BMI, CT imaging provides precise measurements of muscle and fat tissue, which have distinct impacts on prognosis. Low skeletal muscle mass (SMA) and high visceral fat ratios have been associated with poorer outcomes, whereas higher skeletal muscle index (SMI) correlates with improved survival rates.
Serum tumour markers (STM), such as CEA levels, are also crucial in prognostic assessment, indicating higher risks of recurrence and worse survival outcomes when elevated pre-operatively. Combining CT-derived body composition metrics and STM could potentially enhance predictive accuracy beyond individual markers. For instance, studies have shown that models integrating parameters like skeletal muscle density (SMD) and specific tumour markers (e.g., CA72-4) achieved high predictive value for overall survival (OS).
While some models combining these factors have been explored primarily in rectal cancer cases, their broader application across CRC patient populations remains underdeveloped. The proposal of a novel prognostic score integrating body composition metrics and STM aims to address this gap, potentially offering a more tailored approach to predicting outcomes and guiding personalised treatment strategies for CRC patients.
Integrated Prognostic Analysis of Colorectal Cancer Patients Undergoing Surgical Resection: A Retrospective Cohort Study
This retrospective cohort study focused on colorectal cancer (CRC) patients who underwent curative surgical resection at two hospitals between 2017 and 2022. The study included 245 patients in the training dataset from the Second People’s Hospital of Hefei and 120 patients in the external validation dataset from the First Affiliated Hospital of Shihezi University. Inclusion criteria encompassed age 18 years or older, pathologically confirmed CRC, and pre-surgery abdominal CT scans. Exclusion criteria excluded emergency cases, multiple metastases, incomplete data, and absence of neoadjuvant therapy. Clinical data such as gender, age, BMI, tumour characteristics, TNM stage, and tumour markers were collected, with follow-up until 2023 to assess overall survival (OS) and disease-free survival (DFS).
Quantitative Analysis and Prognostic Modeling in Colorectal Cancer
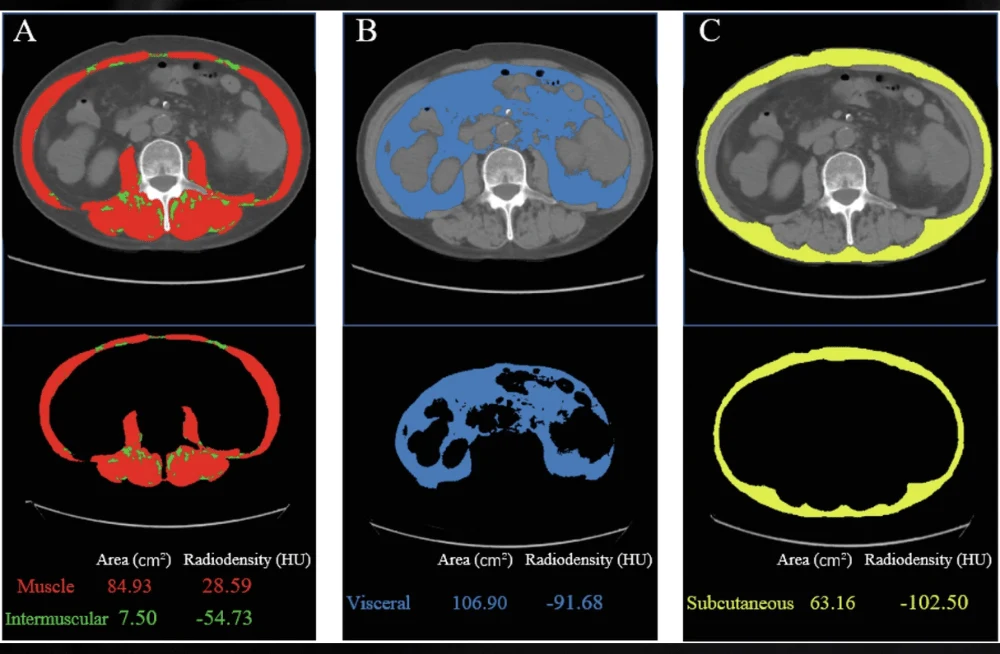
Abdominal CT images, specifically at the third lumbar vertebra (L3), were analysed for muscle and adipose tissue using Tomovision's SliceOmatic software. Skeletal muscle area (SMA), visceral fat area (VFA), subcutaneous fat area (SFA), and intermuscular fat area (IMFA) were quantified based on specific Hounsfield Unit (HU) thresholds. Skeletal muscle density (SMD) and skeletal muscle mass index (SMI) were derived to evaluate body composition. Optimal cut-off values for these indices were determined separately for males and females using ROC curve analysis.
Statistical analyses included chi-square tests, Fisher’s exact tests for categorical variables, Kaplan-Meier curves with log-rank tests for survival analysis, and Cox proportional hazards models for identifying independent prognostic factors. A scoring system was developed based on poor prognostic factors identified from multivariate analyses, and its predictive performance was compared to individual metrics and TNM stage using ROC curve analysis. IBM-SPSS and R software were used for data analysis, with significance set at p < 0.05. Ethics approval was obtained, and patient confidentiality was strictly maintained throughout the study.
Prognostic Factors in Colorectal Cancer: Insights from Body Composition Metrics and Serum Tumor Markers
This retrospective cohort study involved 245 patients in the training set and 120 patients in the external validation set, who underwent curative surgical resection for colorectal cancer (CRC) between 2017 and 2022. The study explored various prognostic factors including body composition metrics and serum tumor markers (STM).
In the training set, patients with higher survival rates were more likely to have colon tumours (p = 0.011), earlier TNM stages (p < 0.05), lower visceral fat area (VFA), lower subcutaneous fat area (SFA), and higher skeletal muscle density (SMD) (all p < 0.05). Higher levels of CEA, CA19-9, AFP, and CA125 were associated with worse prognosis (all p < 0.001). Multivariate analysis identified higher SFA (HR = 0.555, p = 0.029) and higher SMD (HR = 0.527, p = 0.020) as significantly correlated with better overall survival (OS), while high CEA (HR = 1.909, p = 0.008) and AFP (HR = 1.770, p = 0.039) levels indicated poorer OS.
For disease-free survival (DFS), high intermuscular fat area (IMFA) (HR = 1.769, p = 0.033) and high CEA levels (HR = 2.207, p = 0.009) were independently associated with worse outcomes. Kaplan-Meier survival curves confirmed these findings, showing significant differences in OS and DFS based on CEA, AFP, SFA, SMD, and IMFA levels.
To predict OS and DFS, separate scoring systems were developed based on these factors, assigning scores ranging from 0 to 4 for OS and 0 to 2 for DFS. Higher scores correlated with poorer survival outcomes in both the training and validation sets (p < 0.001). ROC curve analysis demonstrated that the new index score had superior predictive ability for OS (AUC = 0.708 in training, 0.698 in validation) and DFS (AUC = 0.668 in training, 0.628 in validation) compared to individual biomarkers like CEA and AFP, as well as TNM stage (all p < 0.001).
Integrated Scoring System Combining Body Composition and Serum Markers Predicts Survival in Colorectal Cancer Patients
This study established a novel scoring system using body composition measures and serum tumour markers (STM) to predict the postoperative survival of colorectal cancer (CRC) patients. The system's predictive efficacy was analysed and compared with single indicators in both a training set and an external validation set, demonstrating its significance in evaluating prognosis and guiding adjuvant therapy strategies for CRC patients undergoing surgical treatment.
The study highlighted the utility of CT-based quantitative body composition analysis, which provides detailed data compared to traditional indicators like BMI or waist-to-hip ratio. Specifically, high subcutaneous fat area (SFA) and visceral fat area (VFA) were associated with better overall survival (OS), aligning with previous findings indicating adipose tissue as an independent prognostic factor in cancer. Conversely, low skeletal muscle density (SMD) correlated with poorer OS, reflecting its role in indicating muscle atrophy and potentially adverse prognosis in CRC patients.
Elevated levels of serum markers such as CEA and AFP were identified as independent adverse prognostic factors for OS in CRC patients, further validating their role in predicting disease outcomes. Combining these markers with significant body composition variables, the novel scoring system demonstrated superior predictive accuracy for OS and disease-free survival (DFS) compared to individual biomarkers or TNM staging alone.
The scoring system facilitates straightforward conversion of continuous variables into categorical scores, enabling clinicians to assess prognosis effectively. Unlike complex nomograms used in previous studies, this system offers simplicity and clinical applicability, enhancing its utility in routine practice. Despite limitations such as the retrospective nature and limited sample size, the study's strengths include its real-world data applicability and demonstration of high predictive performance across different patient cohorts.
Combining body composition metrics from CT scans with STM in a scoring system is a valuable tool for personalised treatment decisions and prognosis assessment in CRC patients post-surgery. This advancement contributes to more precise clinical management and early intervention strategies, thereby improving patient outcomes.
Source & Image Credit: European Radiology