Medical imaging has significantly improved the surgical management of primary hyperthyroidism (PHPT). Accurate localisation of the parathyroid adenoma (PTA) through cross-sectional imaging enables minimally invasive parathyroidectomy (MIP) to be performed on an outpatient basis, avoiding the need for more invasive in-house bilateral cervical exploration (BCE), which is reserved for cases with negative or inconclusive imaging. MIP offers better cure rates and fewer complications compared to BCE, along with shorter operative times, reduced hospital stays, lower costs, and better cosmetic outcomes.
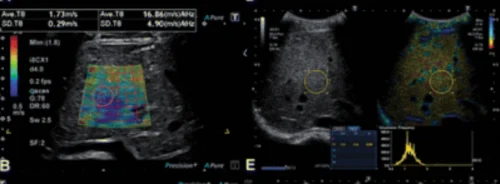
F18-choline (FCH) PET/CT is an emerging 3D nuclear medicine technique showing promise for preoperative localisation of PTA in PHPT patients. It has demonstrated superior detection rates and diagnostic performance compared to the standard Tc99m-MIBI (MIBI) SPECT/CT in several phase 2 clinical trials and a recent network meta-analysis. The benefits of FCH PET include faster study protocols, better spatial resolution for detecting small adenomas, and lower patient exposure to ionising radiation.
However, the role of FCH PET in initial surgical management is still unclear. It is not yet a first-line imaging technique due to lack of market authorisation for parathyroid imaging, higher costs, and limited availability. Although it shows superior diagnostic accuracy over MIBI SPECT/CT, the clinical impact of this difference remains to be fully understood.
The APACH2 trial was designed to compare first-line FCH PET/CT with MIBI SPECT/CT to determine the best imaging modality for achieving successful MIP and normalising calcium levels in PHPT patients requiring parathyroidectomy.
Phase 3 Trial Comparing FCH PET/CT and MIBI SPECT/CT
The study conducted from November 2019 to May 2022 was a multicenter, 2-arm diagnostic intervention randomised phase 3 trial involving four hospitals in Normandy and Brittany, France. It aimed to evaluate imaging techniques for primary hyperthyroidism (PHPT) requiring surgical intervention. Participants, aged 18 and older with confirmed PHPT and no history of certain conditions (previous parathyroid surgery, multiple endocrine neoplasia type 1, pregnancy, breastfeeding, allergies to MIBI or FCH), were eligible. Ethical approval was obtained from the Local Medical Ethics Committee South-East II and the French Agency for Medical and Health Products Safety in 2019, adhering to the Declaration of Helsinki and CONSORT guidelines. Patients provided written informed consent before enrollment.
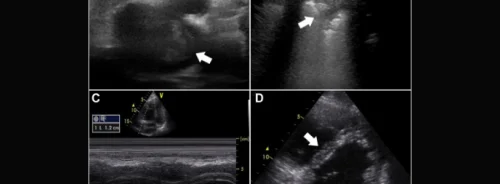
Randomisation was performed in a 1:1 ratio using a web-based system to assign patients to either receive FCH PET/CT (experimental arm) or MIBI SPECT/CT (standard arm). Before randomization, baseline assessments included clinical examinations, neck ultrasonography, and laboratory tests (serum calcium, parathyroid hormone, etc.). Imaging procedures varied based on randomisation: FCH PET/CT for the experimental arm and MIBI SPECT/CT for the standard arm. In cases of negative or inconclusive initial imaging, patients underwent crossover imaging.
Blinded Interpretation and Surgical Outcomes
Interpretation of imaging results was conducted in a blinded manner by two experienced nuclear medicine physicians, with a third review in cases of discordance. Surgical procedures were performed within 12 weeks post-imaging, with outpatient minimally invasive parathyroidectomy (MIP) for positive imaging results and inpatient bilateral cervical exploration (BCE) for negative or inconclusive results. Surgical outcomes, including complications and vocal cord function, were monitored.
Histological confirmation of parathyroid tissue was obtained during surgery, with final analysis based on paraffin wax-embedded sections. Follow-up assessments occurred at 1 and 6 months post-surgery, focusing on clinical and biochemical parameters.
The primary outcome measured the success of first-line imaging-guided MIP in achieving normocalcemia (serum calcium ≤10.2 mg/dL) one month post-surgery. To achieve sufficient statistical power, a sample size of 58 patients was planned, with statistical analyses conducted using R software.
Clinical Outcomes and Safety Profiles
During the study conducted from November 2019 to May 2022, a total of 59 eligible patients consented to participate. Out of these, 57 patients underwent first-line imaging: 29 were assigned to FCH PET/CT (FCH1) and 28 to MIBI SPECT/CT (MIBI1). Baseline characteristics were similar between groups across participating centers.
First-line imaging identified positive results in 24 patients in the FCH1 group and 18 in the MIBI1 group. Patients with negative or inconclusive results underwent crossover imaging: 5 from FCH1 underwent MIBI2, and 10 from MIBI1 underwent FCH2. Surgical procedures were performed accordingly, with outpatient minimally invasive parathyroidectomy (MIP) for positive imaging results and inpatient bilateral cervical exploration (BCE) for negative or inconclusive results.
The primary endpoint, assessable in 27 patients from FCH1 and 25 from MIBI1, showed that 85% of patients in the FCH1 group achieved normocalcemia (mean 9.12 mg/dL) compared to 56% in the MIBI1 group (mean 9.32 mg/dL), indicating a 29% difference (95% CI, 4%-51%).
Secondary outcomes included second-line imaging results: in FCH1, positive MIBI2 scans led to successful outcomes, while in MIBI1, positive FCH2 scans similarly resulted in successful surgeries. Histological examination confirmed parathyroid adenomas (PTA) in most resected specimens, with mean lesion size similar between groups.
The sensitivity of FCH1 was 82% (95% CI, 62%-93%) and MIBI1 was 63% (95% CI, 42%-80%), while positive predictive values were 92% (95% CI, 72%-99%) for FCH1 and 100% (95% CI, 77%-100%) for MIBI1. Follow-up at 1 and 6 months confirmed sustained normocalcemia in most patients who achieved it post-surgery.
Agreement between reporters on imaging results was high (κ = 0.81 for FCH1 and κ = 0.86 for MIBI1). Safety profiles were favorable, with no adverse events related to FCH administration reported, and transient events related to surgery and anesthesia were observed in a few cases.
FCH PET/CT is a promising first-line imaging modality for localising parathyroid adenomas
The clinical trial findings indicate that FCH PET/CT is a promising first-line imaging modality for localising parathyroid adenomas (PTA) in patients with primary hyperthyroidism (PHPT) requiring surgery, potentially replacing MIBI SPECT/CT. Compared to MIBI SPECT/CT, FCH PET/CT showed superior sensitivity, leading to a higher rate of successful minimally invasive parathyroidectomy (MIP) and achieving normocalcemia one month post-surgery.
This study builds on existing evidence of FCH PET/CT's diagnostic superiority over MIBI SPECT/CT in PHPT, focusing uniquely on its clinical impact as a first-line diagnostic tool rather than as a secondary imaging method. The crossover design of the study reinforced the efficacy of FCH PET/CT in second-line imaging scenarios compared to MIBI SPECT/CT.
Strengths of the study include its multicenter randomised phase 3 design, which directly linked diagnostic accuracy with therapeutic outcomes. This approach allowed for assessing the clinical utility of FCH PET/CT in guiding successful and minimally invasive surgical interventions, thus benefiting patients with PHPT by minimizing complications and optimising cosmetic outcomes.
Limitations include the study's relatively small sample size and short follow-up period of six months post-surgery, which precluded long-term assessments of treatment efficacy. Additionally, the study did not assess parathyroid hormone levels as an endpoint, focusing instead on serum calcium levels as a surrogate marker for surgical success.
These findings support the use of FCH PET/CT as a safe and effective imaging tool in the preoperative management of PHPT, potentially influencing future clinical practices and regulatory decisions regarding its widespread adoption in this patient population.
Source Credit: JAMA Otolaryngology-Head & Neck Surgery
Image Credit: iStock