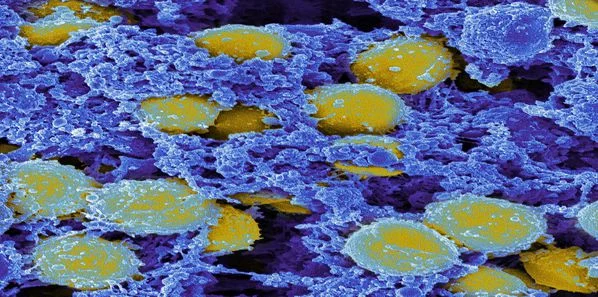
There is no doubt that blood culture isolates are the cornerstone of adequate antibiotic treatment but it is a fact that many blood cultures are contaminated with bacteria residing on the skin. The most common of these contaminants are coagulase-negative staphylococci (CoNS).
Contaminated cultures are
generally discarded and disregarded, but the fact is that these cultures can
provide important diagnostic information such as antibiotic resistance profiles
of CoNS contaminants and those of the actual infecting bacteria isolated subsequently
from the same patient.
Scientists at the
Sackler Faculty of Medicine in Tel Aviv, Israel recently conducted a study on patients
with positive cultures from 2009 to 2012. The study has been published in the
Journal of Antimicrobial Chemotherapy.
Approximately 30
percent of all positive hospital blood culture samples are discarded every day
because they are contaminated. This study shows that rather than discarding
these compromised samples, clinicians can use the resistance profiles of skin
bacteria to treat patients more effectively and to prescribe them antibiotics
that would be more appropriate to their ailment.
The study consisted of
2,518 patients with 5,290 blood cultures. Out of this sample population, 1,124
patients had 1,664 blood cultures with CoNS contaminants. Study data included patient demographics,
patient hospitalisation records, comorbidities, blood culture results and dates
of death.
With respect to the
blood cultures, high overall CoNS resistance predicted high overall resistance
for Gram-positive and Gram-negative bacteria. The resistance of CoNS
contaminants to a specific antibiotic predicted the resistance of the bacterial
isolates to that antibiotic. Highly resistant CoNS isolates were associated
with higher-short term mortality.
The study team found
that most hospital patients are treated at the outset with broad spectrum
antibiotics. These antibiotics are then replaced with more precise
narrow-spectrum antibiotics after a few days when the initial test results are
known to the clinicians. The narrow-spectrum antibiotics are better than
broad-spectrum antibiotics because they treat the specific bacteria. In
addition, broad-spectrum antibiotics can also alter the bacterial environments of
the skin and gastro-intestinal tract as well as promote inflammation and
resistance to pathogens.
According to Gideon Y.
Stein, MD, PhD and lead author of this study, "“Because we have found a
direct correlation between resistance profiles of CoNS contaminants and those
of the actual infecting bacteria isolated from the same patient, the results of
these “junk” samples can be used to predict patient mortality and correct
empirical antibiotic therapy. This should serve as an additional, non-invasive, diagnostic tool.”
Source: LabMedica
Image Credit: Flickr.com