HealthManagement, Volume 5 / Issue 3-4 / 2010
Authors:
Dallas Knight
University of Otago
Sarah Stewart,
Otago Polytechnic
Dunedin, New Zealand
Information and
communication technologies (ICT) present midwives with new opportunities. This
article reviews how New Zealand midwives currently use technology in their
practice, and its implications – both for midwives as well as health consumers
and health organisations. It also discusses where midwives need to develop in
their use of technology in order to meet the needs of the women and families
they work with, and provide evidence-based midwifery care.
Midwives, on the one hand, see themselves as face-to-face, hands-on
practitioners whose role it is to protect women from the interventions of
clinical technology, which they see as increasing poor outcomes for mothers and
babies. On the other hand, midwives recognise the potential for IT to make
their working day easier and improve their practice management, information
management, and communication. Midwives see the need to maintain 'hands-on'
skills and protect normal, nontechnical birth, yet leverage technology to
provide a seamless service at an organisational and professional level.
In New Zealand, midwives use technology for six main purposes; clinical practice, practice management; access and disseminate evidence-based information; communicate with clients (mothers and their families); education, and ongoing professional development.
Midwifery in New Zealand
New Zealand is a small country with a population of just under 4.5 million. Official statistics report approximately 64,000 registered live births in 2009, with an infant mortality rate of 5.0 deaths per 1,000 live births.
According to the Ministry of Health’s Draft Maternity Action Plan 2008-2012, most women (97.5 percent) give birth in a hospital or birthing centre with approximately two thirds having a normal birth, nearly 25 percent are caesarean section with the remainder having assisted vaginal delivery. Nearly all births have a midwife in attendance either as the lead maternity carer (independent midwife) or core (hospital) midwife.
The New Zealand maternity service is funded by central government and free to women. Every woman is entitled to a lead maternity carer (LMC) who is responsible for the woman’s care from conception to six weeks following the birth of the baby. Over 80 percengt of women choose midwives as their LMC.
Midwife LMCs are responsible for planning and implementing women's care; providing information to women so they can make informed choices about their care; organising screening tests such as ultrasound scans; prescribing pregnancy-related medications and referring to other health professionals at appropriate times. LMC midwives may be employed by organisations such as hospitals, or self-employed and paid directly by the government. The vast majority of midwives are direct-entry which means they complete a three-year undergraduate midwifery degree and are not required to be nurses.
In 2009, according to data from the Midwifery Council of New Zealand, 2,652 midwives renewed their annual practising certificates. Approximately half of practising midwives work as LMCs. Others work as core midwives.
Core midwives staff facility and hospital maternity units. They work shifts and provide support to LMCs; care for women once they have had their babies, and provide secondary and tertiary care to sick mothers and babies.
Clinical Practice
Telemedicine does not figure in the provision of maternity care in New Zealand. At most, midwives in rural and remote communities will consult with secondary or tertiary units by telephone or fax.
If more sophisticated monitoring is required of a woman or baby, the woman will be transferred from her home locale to a bigger medical centre.
Practice Management
LMC midwives provide woman/patient centred care in collaboration with other health services including laboratory, radiology, secondary care and other primary healthcare providers such as smoking cessation services. Referrals and information transfer between health professionals (especially between midwives) and institutions are often necessary. At present this information is transferred in a variety of ways but mostly it is not within a standardised secure electronic environment. Paper and faxed information transfer is most often used.
Midwives in different parts of the country may manage their practices differently. It is less common for midwives to receive electronic laboratory results that can be associated with a woman’s electronic record and it is not usual to have referral letters between management systems. While it is possible for midwives to use any of the three commonly used practice management systems to send letters and receive encrypted electronic information such as laboratory results and radiology reports, uptake depends on individual midwives buying into these services. Once the woman’s clinical information is in the system, it is used primarily for statutory record keeping requirements, audit and claiming.
LMC midwives claim fees from a central government funding body in four segments: antenatal services are paid in two units; birth services fees are another fee unit; postnatal care is the fourth fee unit. If compulsory data fields are completed during the maternity pathway, electronic claiming is a straightforward process.
Data is commonly forwarded electronically to an intermediary body, and then fees are claimed on their behalf from the central government funding body. Individual midwives may make their own claim but this is by comparison a lengthy manual process.
At present, most of the electronic systems used by LMCs do support fast, easy and useful clinical information sharing. However, the functions of claiming and easily printed information required for professional accreditation and audit are highly utilised and valued by midwives
Midwifery Information Systems
At a regional level, most secondary and tertiary hospitals now use one clinical maternity database which is capable of becoming a national database. This software provides a system to manage patient information through antenatal, perinatal and postnatal provision, with the ability to generate an extensive range of reports from clinical data. The majority of core (hospital-based) midwives enter booking data into this regional system.
There are also stand-alone maternity databases with neonatal and perinatal information. All pregnancies are recorded in the Maternity and Newborn Information System (MNIS) collection.
Extensive data collection and duplication of data entry is a time consuming and sometimes frustrating aspect of midwives' work. Frequently they do not have clerical staff to enter data, and they do not find the information systems they use to be intuitive.
Recent Health IT Initiatives
The New Zealand National Health IT Board has recently released a plan enabling an integrated healthcare model that will provide a core set of personal health information available electronically to the patient and healthcare providers, regardless of the setting.
The driving force is a vision of person-centred healthcare, which has not been possible because of the mostly disparate and fragmented information systems currently in place. Early adoption and successful use of isolated systems has slowed adoption of a nation-wide health information system that is aiming to be sector owned and community supported.
The New Zealand National Health IT architecture will make it possible for individual systems used by midwives, to access essential core patient information.
Access to Evidence-Based Information
It is vital that midwives have access to quality, evidence-based information for clinical practice in an era of increasing litigation and surveillance by media and other professions. It can be difficult for midwives in New Zealand to keep up top date with the latest evidence. Paper journals have expensive subscriptions, and many hospitals and maternity units are poorly resourced with appropriate journals and textbooks.
The Internet has become very important as a means to access evidence-information. Many hospitals provide access to relevant online databases such as CINALH and Pubmed but fire-walls prevent midwives accessing local hospital library electronic resources from outside the hospital.
The New Zealand Ministry of Health provides free access to the Cochrane Database for all citizens and midwives are able to use these systematic reviews. Nevertheless, midwives find it difficult to access other online journals, unless they are enrolled students at educational institutions, or are prepared to pay the fees that are charged for articles.
Communication with Clients
The Midwifery Council of New Zealand provides a web-based resource (www.midwiferycouncil.org.nz) for consumers to check the current registration details of midwives, and the New Zealand College of Midwives' website (www.midwife.org.nz) lists a set of consumer expectations it considers useful for a woman to consider. Some midwives have a personal or practice website outlining their location, style of practice and contact details but this is not usual. Women frequently have to choose a midwife from a list of telephone numbers.
New Zealand midwives are increasingly using text messaging (SMS) with their patients, not only for appointment reminders but also for clinical questions, and sometimes for support and reassurance. Women offered text communication with their LMC appreciate easy access and support. Nevertheless, midwives have yet to fully implement the specialised software that can document text encounters and download them to a laptop/PC to attach to the woman’s clinical record.
Education: The Virtual Birth Unit
Undergraduate and postgraduate midwifery education in New Zealand has moved to online and blended delivery as a means to addresses a national shortage of midwives. Historically, women have not been able to study to be midwives because they have been unable to uproot their families and move to campus for three years.
Blended and online delivery using a mix of face-to-face intensive workshops, and online delivery of theory allows women to stay in their communities as they study, and encourages them to stay once they are registered. This has become a very important recruitment and retention strategy for rural and remote areas that struggle to retain staff.
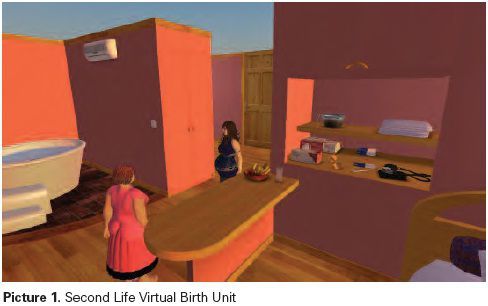
New innovations for education are being piloted, such as the Virtual Birth Unit in Second Life, which was developed by the Second Life Education New Zealand team in 2009 (slenz.files.wordpress.com/2010/03/slenz-final-report-_milestone- 2_-080310cca.pdf).
This virtual simulation supports midwifery students to work through the scenario of caring for a woman in labour and birth. Unfortunately, there are a number of barriers that have prevented this technology to be taken up by educators in New Zealand, including time constraints for up-skilling staff and student as well as institutions' reluctance to make Second Life available on computers because of concerns about security. Nevertheless, there has been a lot of international interest, and American and British midwifery educators are taking up the project.
Professional Development: E-Learning and
Videoconferencing
All New Zealand midwives are required to undergo a rigorous accreditation process in order to practice midwifery. This includes acquiring professional development points relating to professional and education activities. Many midwives find it difficult to attend face-to-face conferences, seminars or workshops because of geographical distance and financial constraints, or they have difficulty in finding time to get away from their practice or employment. With this in mind, education providers are making opportunities for professional development available online.
One example is the “Immunisation eLearning Course” (www.learnonline.health.nz) funded by the Ministry of Health.
This provides professional development points once the midwife has completed and 'passed' the course. There have also been moves to provide professional development opportunities via video conferencing. 'The Telepaediatric Service' video conference network has provided several seminars for rural midwives but as yet these have not become a regular occurrence.
Online informal professional activities, discussions and communities of practice are increasing. Midwives' uptake of Facebook for social networking and sharing information is noticeable, and initiatives such as the free online conference “The Virtual International Day of the Midwife” (http://internationaldayofthemidwife. wikispaces.com) are on the rise. However, the issue of lack of skills prevail as well as concerns about digital identity, and an attitude that learning and networking is best done in the face-to-face context.
Issues for the Future: Decision Support
Systems
Midwives' style of practice involves working with consumers to ensure they make informed choices about their care. Besides having ready access to best evidence, clinicians and consumers in midwifery could be helped by decision support systems.
Most women proceed along a predictable temporal pathway towards the birth of their child, and for the weeks following the birth. Along the pathway there are standard points in time where the same decisions have to be made, requiring the same evidence. Therefore standardisation of care and opportunities for the exploitation of electronic mobile applications for commonly experienced situations arise.
Decision-making could be assisted with electronic Decision Support Systems (DSS) for both consumer and clinician. If the DSS were on the Internet, then access via a mobile device with a data services plan would be possible. Some midwives already have a data-services plan on their notebooks/laptops enabling them to remotely access the internet. There are already mobile applications applicable to midwives and women such as ‘due date’ applications, although these are only a guide, as are other computer tools and expert systems. Clinical judgement would always preside.
Will Mobile Technology Provide Solutions?
In New Zealand there are currently cost constraints for consumers using mobile data services, so mobile internet is out of the range of most consumers. Affordable devices and data services enabling the mobile internet will become available in the foreseeable future and be the drivers of change.
Exploitation of mobile solutions will see ubiquitous access to information and data input. Midwives provide care in their clinics, birthing centres, hospitals and homes so could be seen as mobile clinicians. Data input is required in each of these locations. Devices for mobile recording and transmitting information are becoming available and are currently being considered in New Zealand. Convergence of technologies has given rise to such devices as Net books, iPads and smart phones which are all Internet enabled mobile devices capable of capturing and transmitting information. Smart phones are both communication and computing devices and platforms for collaboration across time and distance. Some midwives already are finding 3G phones useful, and as costs lower, increased uptake could be expected.
Web-Accessible Information
Despite cost constraints, many consumers now have broadband and access to the Internet. However, this does not stop some women having difficulty with finding information about local LMCs.
Prior to first contact with a midwife, women need access to information regarding availability and style of practice of local LMCs. If women were directed to an easy to access site with contact and availability details for midwives, this section of the pregnancy and birth journey could be smoothed. Another section of the site could answer frequently asked questions (FAQ), with a growing database of previously asked questions with the answers and a forum with expert (midwifery) input.
At the moment there are commercial sites providing such services but most consumers and midwives are unaware of, or do not wish to access this service. Consumers who use the registered health professionals are also directed towards other services offered by the professional, which raises questions about the public-private mix and also the degree of sponsorship and advertising accompanying the information and expert help.
Information Needed by Women
Midwives see dissemination of quality evidence-based information as central to the process of informed choice, which is at the heart of the midwives’ contract with women. Consumers need timely, accurate, authoritative information available to them. Currently this is often in the form of printed material given at first consultation and as needed, but further use could be made of trusted internet resources. Besides hardware and broadband services, access to web-based information requires a set of literacy skills. These include: traditional literacy and numeracy, health and information literacy, science literacy and computer literacy. Both women and midwives need these skills to take full advantage of web-based resources.
Women have always valued collaboration and place importance on ‘what other people say’. Consequently there is an increasing trend for women to access social media to take part or follow discussion forums. Online social networking using social media is a comparatively new phenomenon but even so, health groups are already making inroads. Examples are: specialist groups in New Zealand using Facebook, Twitter, Bebo and YouTube to inform and educate mothers on breastfeeding issues (www.facebook.com/breastfeeding ).
This central government backed breastfeeding initiative has a strong online presence. Participation has increased rapidly since the group was established less than a year ago. It is part of a carefully co-ordinated campaign to increase breast-feeding and is a centrally funded initiative.
Conclusion
Midwives need professional, clinical, professional development and administrative information. Services and devices for capturing, accessing, transmitting information have recently improved and availability is accelerating in New Zealand, although midwives are often frustrated by duplication or even triplication of data entry, both paper and electronic.
Midwives would welcome less duplication of data entry as the perceived value to the data collectors (midwives) is sometimes viewed as rather tenuous.
Midwives are also beginning to see the value of eLearning and social media for networking and online collaboration. Online solutions require a skill set, which New Zealand midwifery educators are addressing especially at undergraduate level. Time constraints to developing computer and digital illiteracies are cited but lack of time is due to prioritizing issues down the list, and ways must be found to help clinicians and consumers to use IT.
Collaborative efforts at a national planning level are moving towards more integrated solutions which must be seen as cohesive rather than small and isolated. Systems that are fast, easy and useful to midwives would be welcomed.
� �